Health plans today face both significant challenges and unprecedented opportunities to drive meaningful change. Disparities in care still impact too many, and nearly 9 out of 10 U.S. adults continue to struggle to understand and act on their health information. Yet at the same time, the technology, data, and digital engagement tools available today uniquely position health plans to lead the way and improve the health and lives of millions.
To achieve measurable gains in outcomes, quality, and cost containment, health plans must evolve their engagement strategies and move beyond traditional outreach to embrace AI-powered, equity-centered, behaviorally informed engagement that empowers members to take meaningful action. This evolution must also include intuitive digital experiences: predictive insights, behaviorally informed digital engagement and self-service tools and portals that give members easy access to the resources they need, when they need them, creating trust and reducing friction.
Still, AI is not a magic wand. Its meteoric rise since 2023 and its profound global impact have been extraordinary, but health remains deeply human. Real transformation happens when AI capabilities (like Machine Learning and LLMs) are paired with thoughtful, people-centered program design. Combined with frictionless digital access points, such as mPulse portals
and self-service solutions, health plans can deliver experiences that not only engage but also empower members.
So that is our focus now: a roadmap for health plan leaders to navigate the merging of advanced AI-powered analytics and personalized digital engagement—a combination that creates impact far beyond what each element can do on its own.
DATA, THE IMPERATIVE OF INSIGHT-DRIVEN ENGAGEMENT
In today’s healthcare environment, every transformation begins with data. By harnessing analytics powered by advanced AI technology, health plans can uncover disparities, understand member behaviors, predict what members may do next, and tailor interventions that act on both present realities and future possibilities.
For example, predictive models can identify members at high risk of adverse outcomes and trigger proactive interventions to mitigate risks. When those same members engage through portals or self-service tools (checking lab results, completing a survey, or scheduling a visit), health plans gain additional context. These touchpoints enrich the predictive models, creating a dynamic feedback loop where engagement both drives and improves the data.
COLLABORATING WITH ANALYTICS PARTNERS
 Harnessing this depth of data requires AI and machine learning partners capable of processing hundreds of data points across millions of members, including:
Harnessing this depth of data requires AI and machine learning partners capable of processing hundreds of data points across millions of members, including:
- Historical interaction data
- Claims and clinical utilization patterns
- Eligibility and enrollment data
- Treatment adherence rates
- Public census and socio-demographic factors
- Portal and self-service utilization data
The combination of traditional health data with digital engagement footprints creates a more complete picture of the member journey. For health plans, this means being able to predict not only who is at risk, but also how they are likely to engage, and what digital experiences are most effective in moving them to action.
VENDOR BEST PRACTICES
When selecting analytics partners, consider:
- Data Readiness and Governance: Strong frameworks ensure integrity and compliance while enabling data from portals and self-service tools to be securely integrated into population-level insights.
- Predictive Models and Segmentation: Advanced models should incorporate engagement data, including portal usage, to enhance risk prediction and personalize outreach.
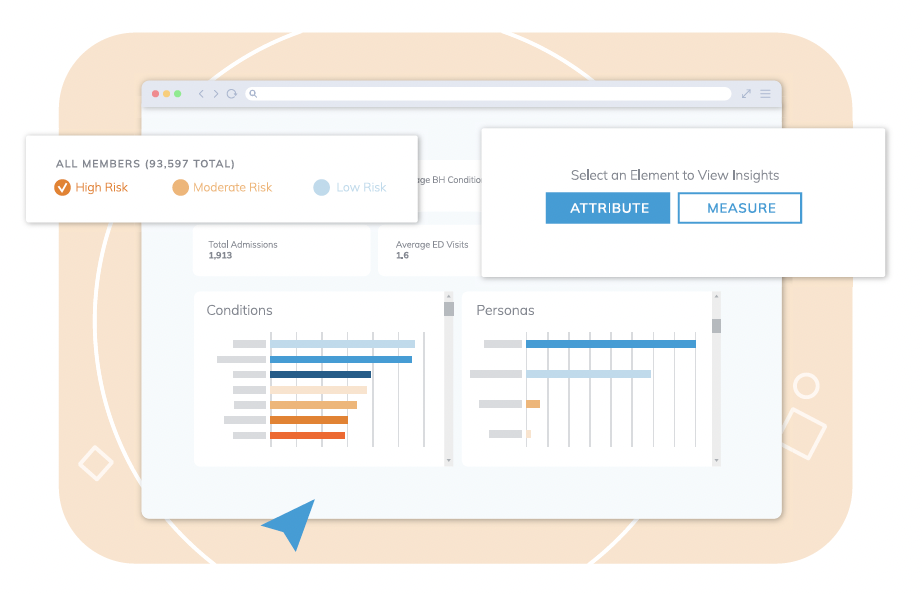
- Interactive Dashboards: Member and population-level dashboards should visualize not only health trends and engagement metrics, but also how members are navigating digital portals, helping reveal barriers, preferences, and opportunities for self-service optimization.
Then, Design Engagement Strategies That Empower, Not Just Inform
While data and analytics provide critical insights, success lies in how health plans translate those insights into strategies that do more than inform—they must empower members to act and sustain healthier behaviors.
Over years of testing and refining engagement across billions of touchpoints, we’ve found that in addition to a strong foundation of data, a successful engagement strategy has a few critical components.
CHANNEL STRATEGY: MATCHING METHODS TO MEMBERS
The power of this channel mix comes not from variety alone, but from alignment and using analytics to match each member with the channels and self-service experiences most likely to drive action and close gaps.
Omnichannel outreach ensures health plans meet members where they are. Whether through text, email, or IVR, the objective is to adapt to the member’s preferred communication channel rather than expecting them to seek out information on their own.
But outreach is only the first step. The most impactful strategies seamlessly direct members into self-service pathways within portals, where they can take action immediately (scheduling appointments, completing assessments, accessing educational resources, or troubleshooting barriers). Portals extend engagement from communication to execution, turning a message into measurable behavior change.
COMMONLY DEPLOYED CHANNELS INCLUDE:
- Text Messaging – quick, direct communication and reminders that maximize engagement.
- IVR and Email – accessible for members with limited digital access.
- Member Portals – deliver rich, interactive experiences that provide access to critical health information, benefits navigation, and personalized resources;
when paired with self-service tools, they deepen engagement and empower self-efficacy.
- Mobile Web – expands access to digital experiences and surveys without requiring app downloads.
- Live Calls – crucial for hard-to-reach members or those who prefer live interaction.
- Direct Mail – valuable for mandatory health communications and digitally limited populations.
TWO-WAY CONVERSATIONS: CONVERSATIONAL AI AND NLP
Two-way conversational capabilities bring scale and empathy to member engagement. Conversational AI and Natural Language Processing (NLP) enable tailored, natural integrations with thousands of members simultaneously though amplifying outreach designed by human experts, at scale.
For example, when a member texts, “I need help finding a doctor,” the system can instantly respond with a link to the portal’s provider finder tool. This is made possible by intelligent Conversational AI and natural language processing (NLP), which interpret the request in real time. Combined with thoughtfully crafted messaging, this approach not only addresses the member’s barrier but also encourages use of the portal—ultimately driving long-term engagement and adoption.

Turning Member Data into Action: A Practical Guide for Health Plans
Real World Use Case: Taking a Look at CAHPS Performance
By integrating predictive analytics with member engagement data, health plans can prioritize
interventions with precision. CAHPS improvement strategies can combine predictive modeling with portal engagement data to identify which members are least likely to respond favorably, and whether they are actively engaging with self-service resources.
For example, a plan could analyze 20,000 CAHPS-eligible members and identify just 2,937 members who would most influence survey outcomes. By layering in portal activity data, plans can further segment this group into those actively engaging online versus those requiring more intensive outreach. This dual approach helps to maximize resources while improving the likelihood of success.
A leading Medicare Advantage plan partnered with mPulse to leverage predictive analytics and Just-in-Time (JIT) outreach to improve CAHPS performance and retention. By using data to identify both the highest-risk members most likely to rate poorly and the lowest-risk members most likely to respond positively, the plan deployed a mix of targeted live calls, motivational mailers, and issue-resolution scripts to influence member sentiment at critical moments.
The program not only improved CAHPS outcomes but also generated substantial retention gains.
Members who received outreach disenrolled at a 2.7x lower rate than those who did not, and the program retained an estimated 186 members, equating to more than $1.1M in financial value over three years.
Overall, the initiative delivered a 776% ROI by year three, demonstrating the power of predictive analytics and data-driven engagement to transform both member experience and plan performance.
Conclusion: A Call to Action for Health Plans
The journey from data collection to delivering equitable, meaningful health impact is both complex and essential. Health plans that prioritize not just the volume of outreach but the quality of engagement, and center members as active partners in their health, will be best positioned to improve outcomes, reduce disparities, and sustain financial health.
The path forward requires leveraging advanced analytics to understand population needs deeply, designing engagement strategies grounded in behavioral science and health literacy, and scaling these efforts with operational efficiency and empathy. Most importantly, it demands a commitment to equity, ensuring every member receives culturally relevant, accessible, and trustworthy support.
To drive this transformation, health plan leaders must build internal alignment across clinical, marketing, operational, and quality teams, fostering a culture of continuous learning and innovation. Equally critical is cultivating strong external partnerships with advanced and innovative technology vendors, community organizations, and care teams, to expand reach and drive impact.
By embracing these priorities and leveraging Health Experience & Insights technology platforms like mPulse, health plans can unlock the full potential of digital engagement: empowering members, improving health equity, enhancing quality metrics, and securing sustainable cost savings.
The time to act is now. Your members are ready to engage. Together, we can create a future where every person has the opportunity to lead a healthier life.






