Quality improvement teams, fresh off the latest Star Ratings release, are again feeling pressure to improve member experience, reduce abrasion, and strengthen Stars performance. Many of the plans we partner with lean on AI and advanced engagement technology to do this successfully—and their results offer valuable lessons for what works.
What’s changing in CAHPS, HOS, and Star Ratings—and what it means for health plans
Health plans are navigating a much tougher landscape than in years past—one where member experience carries as much weight as traditional clinical and operational metrics.
With the bar for earning higher Star Ratings becoming more stringent, every interaction now plays a crucial role in shaping how members feel.
There’s also less room for missteps. With only a small window to influence sentiment before CAHPS and HOS are fielded, the early touchpoints with members matter more than ever. Outreach needs to feel coordinated and respectful of people’s time to avoid abrasion and build trust.

Turning Member Data into Action: A Practical Guide for Health Plans
By using technology that anticipates member needs, identifies barriers, and strengthens communication, health plans can move beyond siloed outreach and create moments that resonate across care experiences.
Member experience is perception-driven, not performance-defined
Even the strongest operational performance doesn’t guarantee strong CAHPS or HOS results. What matters is how members feel when navigating their plan, interacting with service teams, or receiving support. A technically high-performing plan can still underperform if experiences feel fragmented, inconsistent, or impersonal.
 This disconnect reflects the broader “perception versus performance” gap many plans face. Members aren’t asked whether a plan closed a care gap—they’re asked how easy it was to get the care they needed, whether they felt supported, and if their interactions felt clear and respectful. This is where behavioral science becomes especially valuable. Language, timing, and channel all shape member sentiment in vital ways.
This disconnect reflects the broader “perception versus performance” gap many plans face. Members aren’t asked whether a plan closed a care gap—they’re asked how easy it was to get the care they needed, whether they felt supported, and if their interactions felt clear and respectful. This is where behavioral science becomes especially valuable. Language, timing, and channel all shape member sentiment in vital ways.
Small adjustments—like phrasing a reminder more empathetically or reaching out at the right moment—can shift an interaction from feeling overwhelming to supportive.
Personalization also plays a critical role. When messages acknowledge a member’s needs, anticipate barriers, or reflect recent activity, trust increases. And trust is one of the strongest predictors of positive CAHPS and HOS responses.
mPulse’s consumer-centric approach to engagement is built for this reality. By pairing behavioral science with relevant, contextual messaging, plans can improve how members feel throughout their journey, not just how they perform on paper.
From one-off programs to orchestrated member journeys
Today’s health plans need coordinated, connected journeys that prioritize the right message for the right member at the right time.
When different departments reach out independently—each with its own priorities, timelines, and messaging—members often feel inundated or confused. This overlap contributes to abrasion and can undermine the experience plans are working to improve.
 Instead of standalone communications, plans can coordinate outreach across teams so each interaction builds on the last. Unified orchestration delivers consistent communication that reflects a member’s context and reduces unnecessary noise.
Instead of standalone communications, plans can coordinate outreach across teams so each interaction builds on the last. Unified orchestration delivers consistent communication that reflects a member’s context and reduces unnecessary noise.
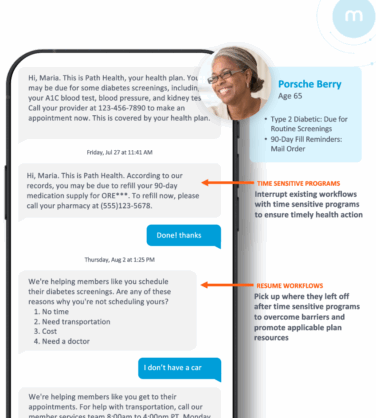
Predictive modeling strengthens this even further. It works by analyzing past behavior, claims patterns, engagement history, and demographic or social risk factors to anticipate what a member may need next.
These models spotlight early signals—such as likelihood to respond, potential barriers, or upcoming care needs—so teams can take action before a member becomes disengaged or frustrated.
This transforms orchestration from reactive outreach into a more proactive, continuous experience. Paired with omnichannel engagement, these insights help plans identify members at risk and prioritize outreach based on impact. This allows teams to focus on programs that meaningfully move the needle.
For a deeper look at how health plans can turn predictive insights into practical, real-world action, explore Turning Member Data into Action: A Practical Guide for Health Plans.
Evaluating outreach through the lens of member experience—instead of just program outcomes—helps ensure your resources support a cohesive journey rather than a collection of disconnected efforts.
mPulse is built to guide this process through an experience-led approach that helps organizations coordinate engagement strategies, break down internal silos, and provide seamless member journeys.
The result? Your teams benefit from a clearer line of sight across all outreach efforts, as well as the ability to sequence messages in ways that feel more coordinated and reduce abrasion.
Discover how mPulse enables connected engagement across channels.
Using data and predictive analytics to target the right members
Data isn’t just something to report on at year’s end—it’s one of the sharpest tools plans have for anticipating risk and guiding outreach. By combining claims, pharmacy, and enrollment data, mPulse identifies the members most likely to benefit from timely support.
These insights highlight moments when a member may be:
- Approaching or overdue for a needed service
- Struggling to navigate benefits or next steps
- Experiencing friction from a recent touchpoint
- Managing behavioral or social barriers that influence their satisfaction
With this visibility, teams can act with greater precision, segmenting and prioritizing in ways that reduce unnecessary contact and reach those who need it most.

Talking CAHPS: The 2025 HOS Edition
Matching outreach channels to member needs at scale
Choosing the right channels is just as important as choosing the right message.
Members engage differently depending on their preferences and circumstances, so plans need an omnichannel approach that meets people where they are and keeps communication well-timed.
 Many plans blend channels such as:
Many plans blend channels such as:
- SMS for quick, convenient touchpoints
- IVR for automated reminders or simple confirmations
- Live calls when a conversation or added reassurance is needed
- Mailers and print for members who prefer traditional outreach
- Portals and mobile tools for self-service navigation
When channels work together, plans can personalize at scale and outreach feels coordinated rather than repetitive.
mPulse’s Omnichannel Engagement Model supports this by using Just-in-Time, data-driven communication at moments when members are most receptive.
Behavioral science also plays a vital role. Timing, tone, and format shape how members perceive each interaction, and thoughtful sequencing helps ensure outreach feels supportive instead of interruptive.
mPulse’s Content Hub reinforces consistency by centralizing approved, behaviorally informed content that can be adapted across channels. This helps teams deliver messages that feel cohesive, intentional, and tailored to each member’s needs.
Transforming engagement into measurable outcomes
Quality improvement teams need evidence, not just strategy. To show real progress on CAHPS, HOS, and retention, plans must connect engagement efforts with measurable results—not only at the end of the year, but throughout the member journey.
One of the strongest ways to demonstrate impact is by linking engagement programs directly to Stars outcomes and ROI.
When plans compare engaged and unengaged populations, clear patterns emerge: members who receive well-timed communication close more gaps and report better experiences.
Teams adjust campaigns in real time, refine messaging, and focus resources where they have the most impact. This keeps operational efforts aligned with what most meaningfully shapes both experience and performance.

Driving CAHPS Excellence: A Health Plan’s Playbook
Ready to Drive CAHPS Excellence? Download mPulse’s Health Plan Playbook for Engaging Providers and Enhancing Member Experience!
What’s next: AI and personalization in quality improvement
AI is creating new ways to personalize at scale by identifying patterns, anticipating needs, and tailoring outreach more precisely than manual workflows allow.
But the real value comes from using these capabilities responsibly, in ways that protect privacy and support member trust.
![]() mPulse applies advanced LLM capabilities within the HXI Platform to create more meaningful, context-aware outreach. AI helps summarize complex member information, surface likely barriers, and suggest message variations—all while maintaining a HIPAA-compliant architecture built for healthcare-grade security.
mPulse applies advanced LLM capabilities within the HXI Platform to create more meaningful, context-aware outreach. AI helps summarize complex member information, surface likely barriers, and suggest message variations—all while maintaining a HIPAA-compliant architecture built for healthcare-grade security.
AI also gives teams breathing room and relieves operational strain. By automating time-consuming tasks, it removes work that often pulls staff in too many directions. This means more time focused on the interactions that truly benefit from human expertise.
These capabilities help teams understand not just what members need, but when and how they’re most likely to engage. This insight enables more tailored experiences without added burden.
As plans look ahead, AI-driven journey orchestration offers a strategic advantage: personalizing interactions at scale while staying aligned with regulatory expectations, resource constraints, and member preferences.
Scaling trust and driving impact
Improving CAHPS, HOS, and retention ultimately comes down to how supported members feel.
A more cohesive, coordinated approach makes this possible. With clearer visibility into member needs, more intentional engagement across channels, and AI-driven insights that reduce operational strain, plans can focus their efforts where they matter most.
mPulse brings these ideas to life with solutions built to meet member needs and support the teams who guide them.
If you’re charting a new direction for CAHPS and member experience, mPulse’s CAHPS & Member Experience solution offers a scalable, practical path to creating a more connected journey.






