From as early as the 16th century, humans have been using the scientific method to collect data points and make decisions based on objective observations. As societal systems have advanced, methods for data collection have also expanded, ranging from surveys, interviews, focus groups, and secondary data analyses. Still, these methods were not designed to adjust for the stratifying systems of our current society—such as ableism, racism, sexism, classism, and colonialism—leaving significant room for error to exclude historically marginalized populations, and in the case of health outcomes, lead to larger health disparities.
We look to data to counter inaccurate beliefs with science and facts. Building a strong evidence base of data has become a precursor to driving important, strategic decisions. Today, data is everywhere. How do we make the most of it?
Principles For Data Equity
The solution is twofold: we must 1. find ways to make the data more representative of the populations being served and simultaneously 2. include the narrative around the data that cannot be collected. For a more equitable dataset, the CDC Foundation’s Principles for Using Public Health Data to Drive Equity provides tools to center equity in the data life cycle, hinging on recognizing and defining systemic factors, using equity-mindedness for language and action, and allowing for cultural modification.
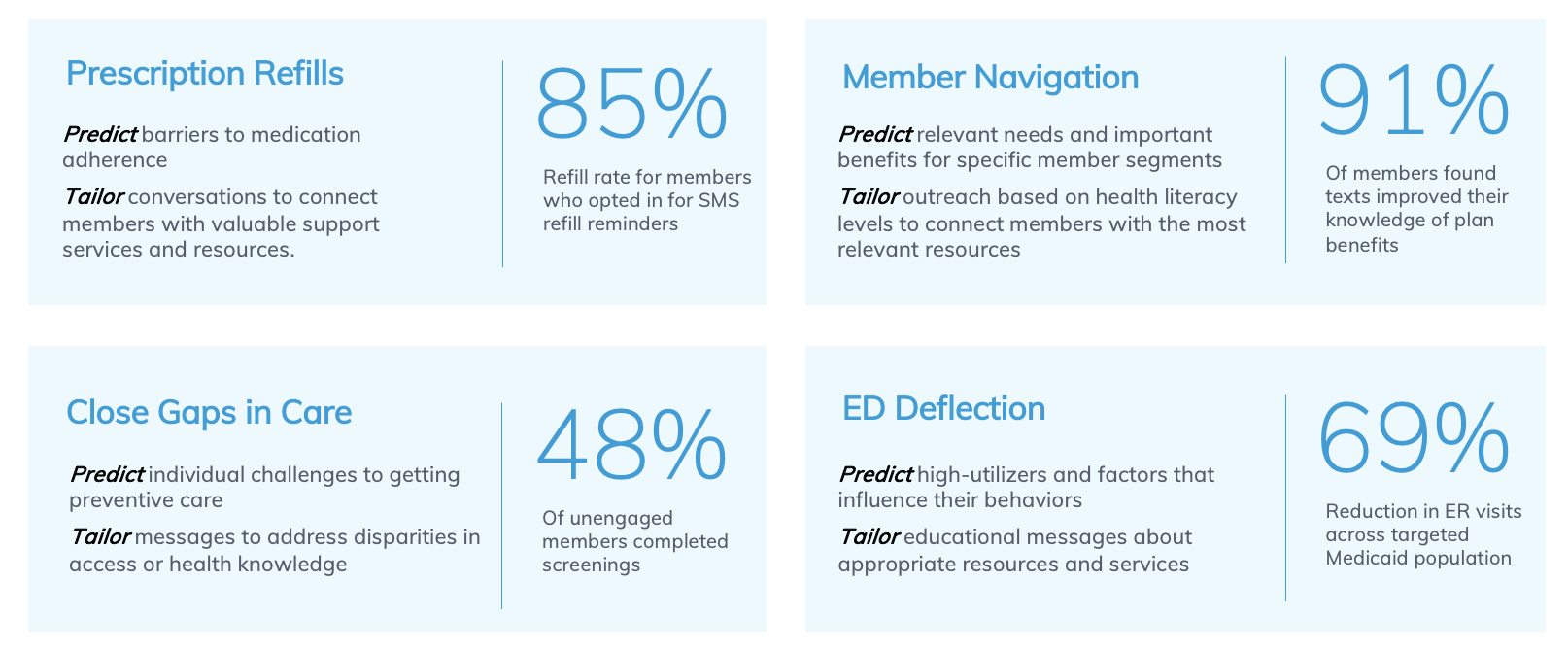
At mPulse, we embed these equitable practices throughout our data lifecycle to bring a focus on health equity, prioritize deeper community engagement strategies, and address the social and economic factors that affect health outcomes.
When Numbers Don’t Tell the Whole Story
When a group is not represented in data collection—whether they are accidentally excluded, non-responsive, or dropped out because they have more barriers to engagement—there is a sampling bias in the data that can have long-lasting consequences for entire communities.
This happens when data is unavailable for a marginalized group and is not accounted for in adjustment methods. It translates into data analyses and reporting, and consequently, excludes these groups from key decisions. This can lead to already marginalized groups being overlooked in program design, policymaking, resource allocation, funding, and more, systemically putting them at an even further disadvantage. Historically, this has led to race neutral policies, such as grandfather clauses, literacy tests, and redlining. When these decisions are made across housing and built environment, education access, economic stability, and food policy they also affect an individual’s overall health outcomes.
An example of this is the race and ethnicity data collection process. As the US population demographic has diversified, the racial designations on surveys have not: all Asians are grouped together along with Pacific Islander. They do not account for the many various identities that exist within these populations. Inclusivity needs to intentionally be built into data collection methods, to ensure that people who are not a part of the demographic majority are also represented within the data.
In a data-driven world, it is crucial to use an equity lens throughout data collection, analyses, and reporting. This can drive better decisions, efficiency, increase revenue, and arguably most importantly, even help lower premature illnesses and preventable deaths.
Overcoming Barriers: Reducing the Burden
Health equity work is a gradual process of undoing harmful, institutionalized rules and making new rules striving toward justice. This begins with making sure everyone’s data points are included:
- Recognizing the barriers that prevent populations from being a part of the narrative and
- Providing means to overcome these barriers
Digital outreach has vastly improved data collection methods—it overcomes multiple barriers such as the time it takes to get to a location, saves on transportation, can offer multiple languages, etc.
Data Equity: Building Trust and Striving to Justice
One barrier that has proved harder to overcome is medical mistrust. Stemming from the adverse treatment dating back to exploitation of enslaved Black bodies to do scientific research, there is a deep-rooted distrust among Black Americans towards medical professionals. This medical mistrust results in underutilization of services, weathering, and missing data. While there is no quick fix, promoting and supporting doctors of color, teaching cultural humility, and updating medical guidelines are a start to building more equitable practices within health systems.
Black and brown patients are now poorly represented in clinical and drug studies, leading to a large data—and knowledge—gap, that translates to misdiagnoses. For example, literature has taught medical professionals what skin symptoms look like on white skin, but have not shown how they may look different on black and brown skin. The missing data points result in missing information and knowledge gaps for providers, subsequently leading to misdiagnoses, and ultimately creating greater health disparities for people with darker skin.
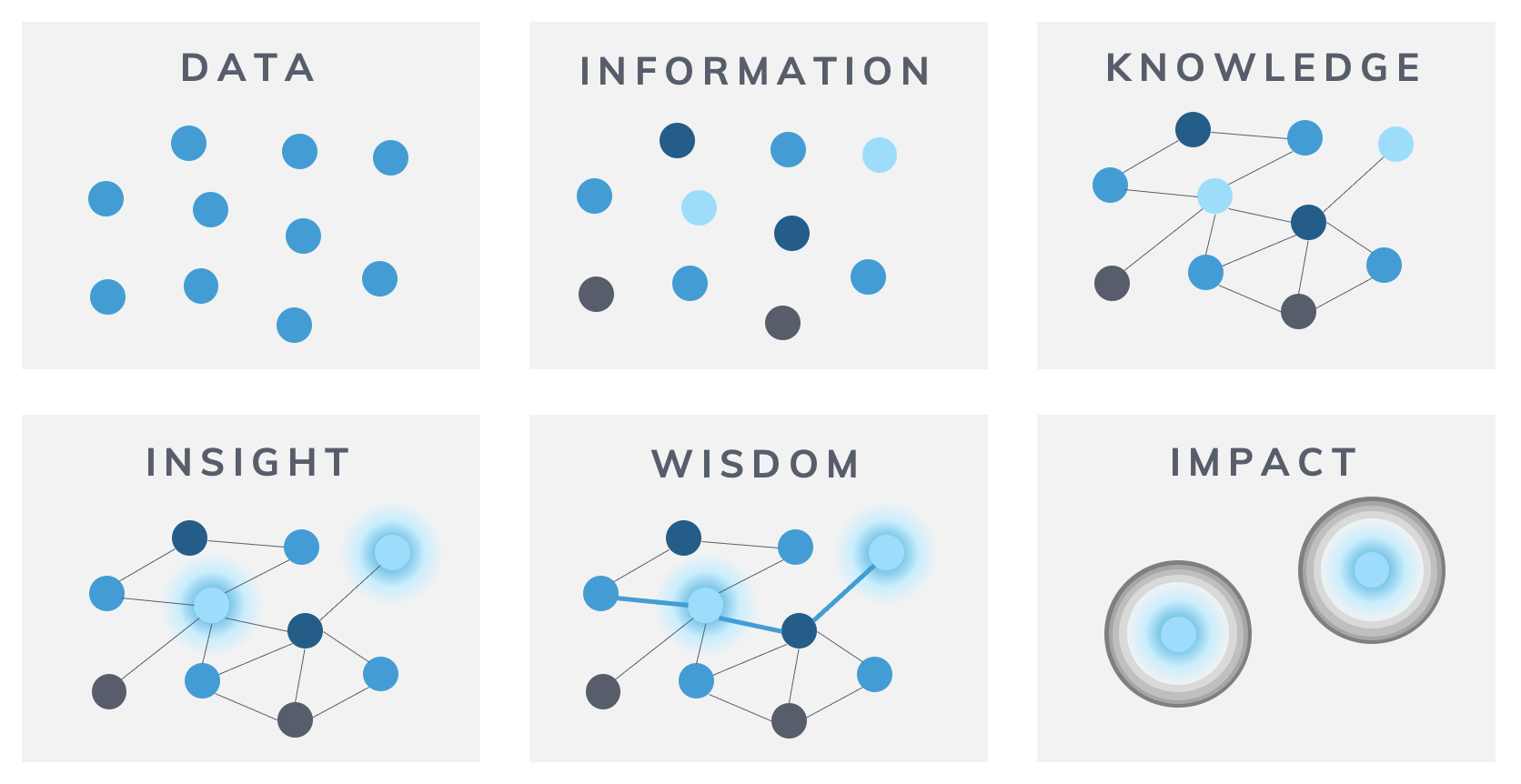
Data to Impact Journey (famously known as Information vs Knowledge)— Source: Gaping Void
When looking at data, we cannot rely on the raw numbers alone. It is equally important to analyze who is not fairly represented and qualitatively share the barriers that have led to their data exclusion. If we cannot remove barriers in data collection, there are other ways to uplift the unheard voices into the overarching narrative. To glean more useful insights from the population trends and patterns we collect, it is critical to understand the context behind the numbers.
Digital Solutions: Practical Approaches to Representational Fairness
Health equity is central to the creation of our HEDIS gap-closure oriented Engagement Solutions: they promote health literacy, demonstrate cultural competency, increase accessibility, and address social determinants of health by:
- Prioritizing health literacy through behavior science and learning strategy to create empowering, actionable language.
- Including creative engaging streaming content assets to supplement and simplify educational messaging.
- Platform-level omnichannel approach increases reach and receptiveness by providing information through multiple digital modalities (SMS, IVR, Email, and streaming health), removing accessibility gaps for people who may be hearing or visually impaired.
- Translations are available for multicultural sensitivity and inclusivity, which improves health literacy and maximizes information retention.
- Cultural competency is built in through natural language understanding available in 7+ languages.
Our engagement strategy intentionally uses data disaggregation to ensure representation of marginalized populations and address social determinants of health (SDoH). Using a proprietary SDoH Index, which leverages a weighting system to maximize its predictive ability, we provide tailored, relevant, and empathetic conversations to members. These solutions are designed to be comprehensive, multilevel, adaptable, and culturally appropriate for populations experiencing health disparities. Insights gained from outcomes can be funneled back into existing Engagement Solutions to provide targeted, relevant outreach to maximize gap closure potential. These tailored digital Engagement Solutions implement an equity-minded approach to close health gaps for groups that have been historically excluded, exploited, and marginalized, and ultimately promote a fair and just opportunity for everyone to reach their optimal health.
To learn more about using digital engagement to build more equitable health data, register for Activate2023: Designing Customer Journeys for Health Equity.