As John Green insightfully notes in The Anthropocene Reviewed, “Disease only treats humans equally when our social orders treat humans equally.”
Yet, daily, we witness the continuation of health inequities through systemic barriers like inaccessible healthcare, disparities in information access, and food deserts.
Our latest white paper, Digital Engagement Strategies to Support Health Equity, provides a comprehensive blueprint for addressing these persistent disparities.
It identifies four pivotal areas ripe for innovation:
- enhancing accessibility
- boosting health literacy
- addressing social drivers of health (SDoH)
- fostering cultural competency
Challenge 1: Accessibility
Accessibility spotlights the basic right of individuals to access healthcare services, a right hindered by transportation challenges, disabilities, language barriers, and systemic distrust. Despite the potential of digital technology to close these gaps, the digital divide leaves 14.5 million Americans without reliable internet, severely limiting access to telehealth services, patient portals, and online appointment scheduling. Yet, with 97% of Americans owning a mobile phone, alternative channels like SMS, IVR, and printed communications hold the key to bridging this divide.
SMS
90% of text messages are read in the first three minutes, and ownership levels remain incredibly high regardless of SDoH factors such as age, income level, ethnicity, or education.
IVR and Print Communication
These are effective channels that don’t rely on internet access and can bridge the digital divide for the portions of your member or patient population that are largely cut off from the digital world.
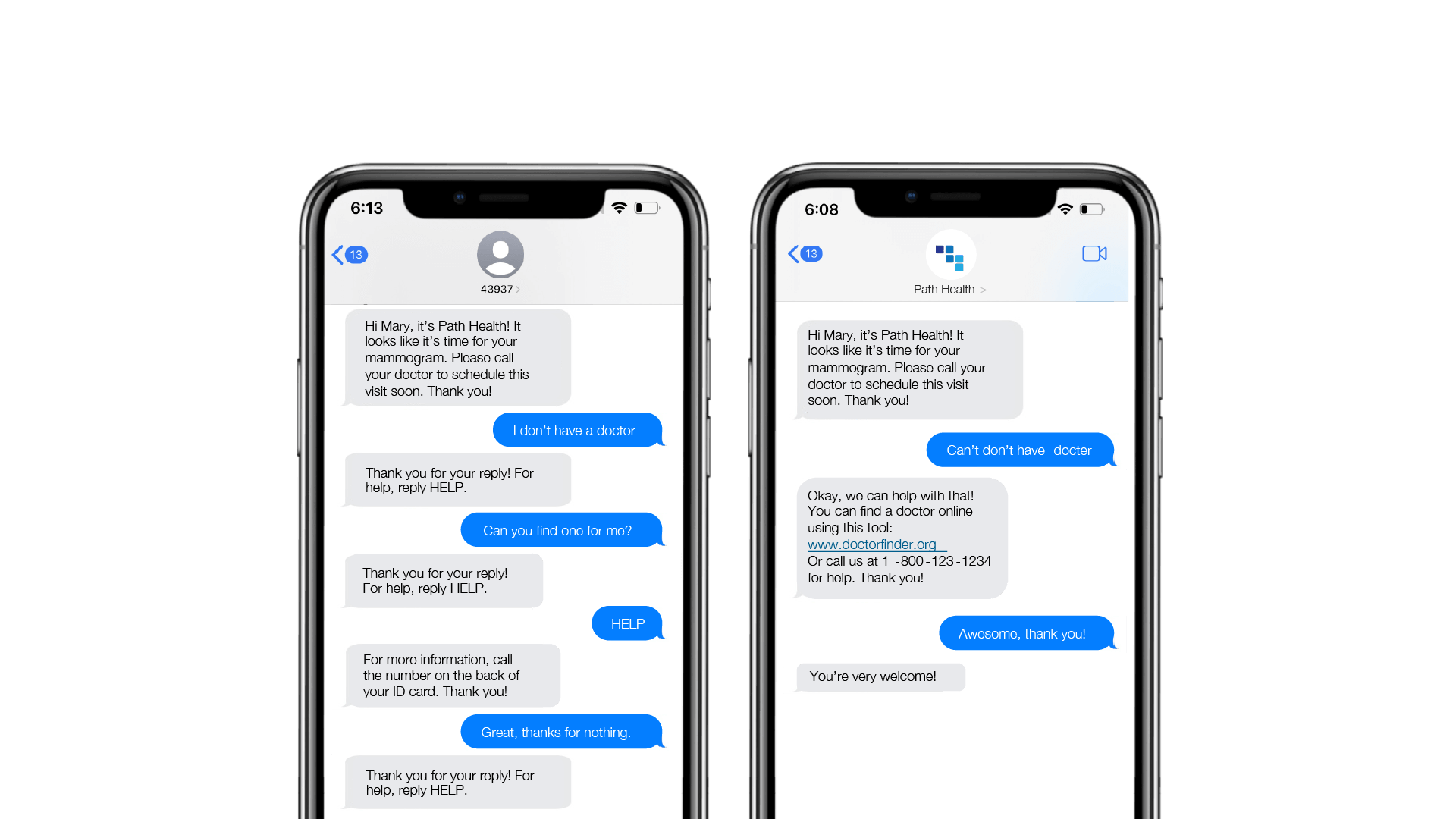
Conversational AI and Natural Language Understanding (NLU)
These technologies offer promising avenues for addressing accessibility challenges. Conversational AI uses technology to interpret and intelligently respond to a message, creating tailored conversations with thousands of people at a time without the need for human involvement. NLU enables computers to understand the intent of a message even if it doesn’t conform to standard, expected responses and to account for typos or off-script responses. NLU allows the interaction with each person to continue in a way that feels familiar, conversational, and natural.
With these two capabilities coupled together, you have a uniquely powerful tool for assessing and breaking down barriers to access on a large scale.
Challenge 2: Health Literacy
Health literacy underlines the critical role of understanding and using health information in making informed health decisions. A staggering $106–$238 billion is added to healthcare costs annually due to inadequate health literacy. Simplifying communication, using clear and actionable language, and employing visuals and stories can make health information more digestible and engaging, thus improving health outcomes and reducing costs.
The way you talk to people matters
For example, almost half of American Adults read below an 8th-grade level, yet health content, on average, reads at a 12th-grade level. When outreaching, we therefore recommend using clear, relatable, readable, and actionable language, defining and breaking down complex terms, and using visuals to make information engaging and understandable.
Pair your learning strategy with technology
Pairing a strong learning strategy with technological capabilities like Conversational AI and NLU allows organizations to identify why individuals aren’t seeking care and deliver engaging, helpful content that will educate and raise their overall health literacy level. For example, the content below shows how you can use streaming content to encourage health actions such as vaccination.
Challenge 3: Social Determinants of Health (SDoH)
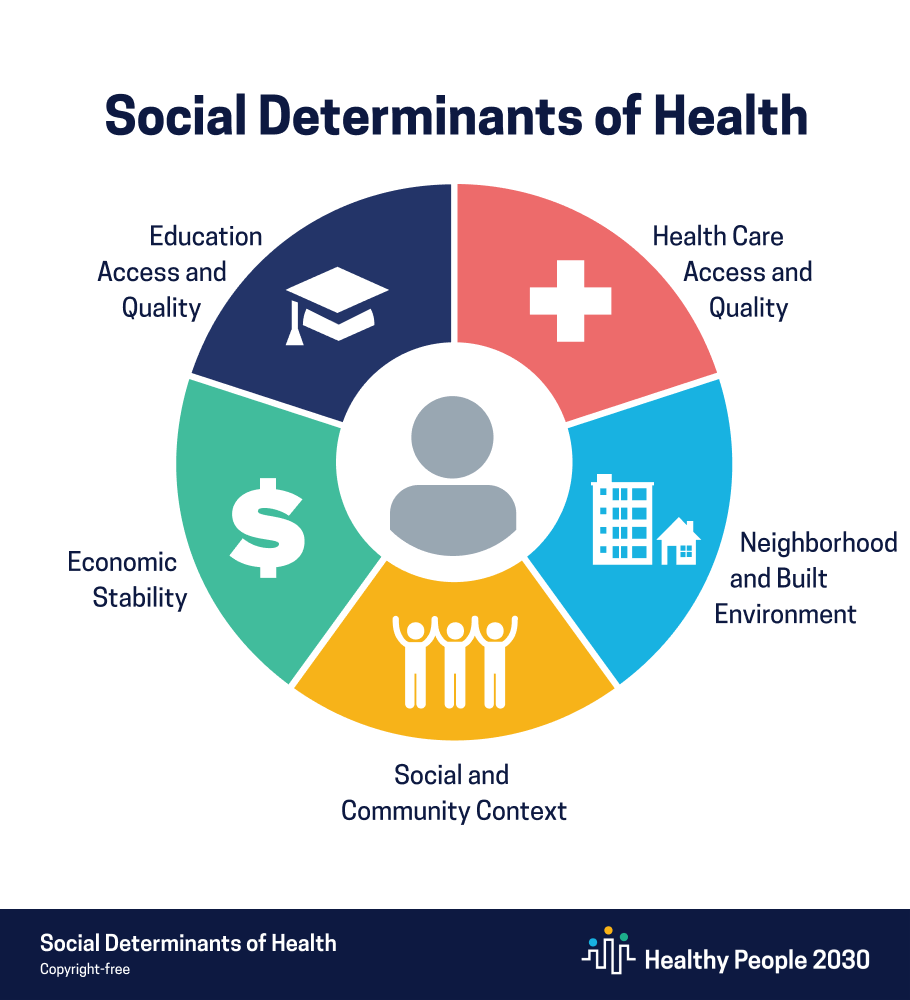
SDoH significantly shape health outcomes, often more than medical care. With socioeconomic status, education level, and ethnicity playing crucial roles in health disparities, employing SDoH indexing and tailored outreach becomes essential in delivering personalized care and resources, effectively addressing the unique needs of each individual.
SDoH Indexing
SDoH Indexing enables healthcare organizations to predict and address individual needs, facilitating tailored outreach and resource allocation.
With Conversational AI and NLU, you can use the SDoH Index to support personalized conversations across your entire population with outreach that is respectful of and responsive to health beliefs, practices, and needs across diverse populations.
Community-Based Resources
Community-based resources are gathered from people’s engagement with these tailored programs. Their responses help to validate the SDoH Index’s predictions and provide deeper insights. Organizations can collect data points from these conversations, which satisfy HEDIS requirements for Race and Ethnicity Stratification (RES), and these data points can be automatically updated in the member profile.
Challenge 4: Cultural Competency
Cultural Competency highlights the importance of inclusivity in healthcare, recognizing the diverse experiences that influence individuals’ interactions with the healthcare system. From ensuring language inclusivity to adopting a stance of cultural humility, healthcare outreach and resources must reflect and respect the rich tapestry of human experience, fostering trust and improving health outcomes across all communities.
Language and Word Choice
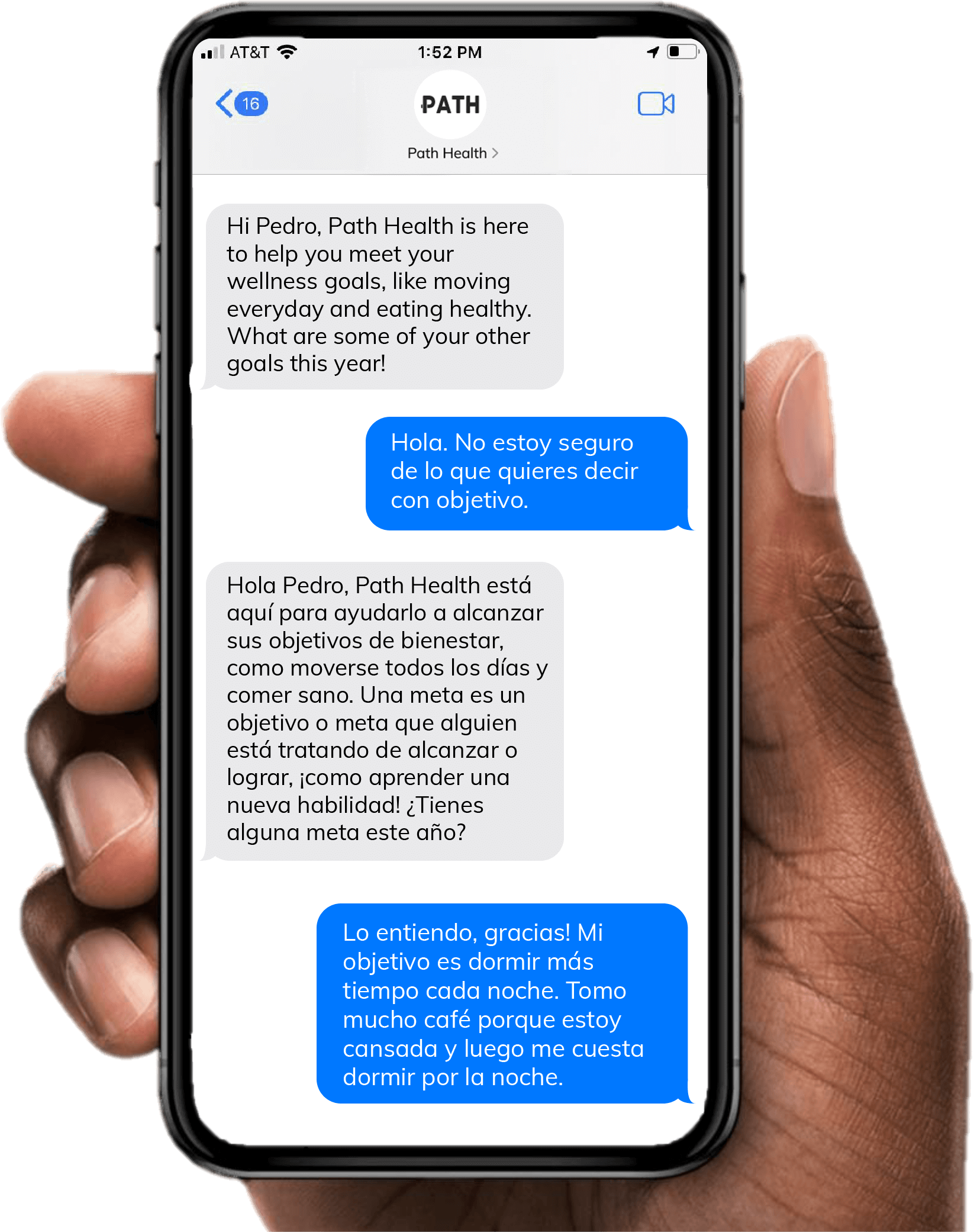
Speaking to your health population in their preferred language is a fundamental practice for cultural competency, as is having the ability to adjust.
However, word choice can also build or erode a relationship. Certain words can trigger distrust or, conversely, show a deeper understanding of an individual’s culture and life.
The Power of Perception
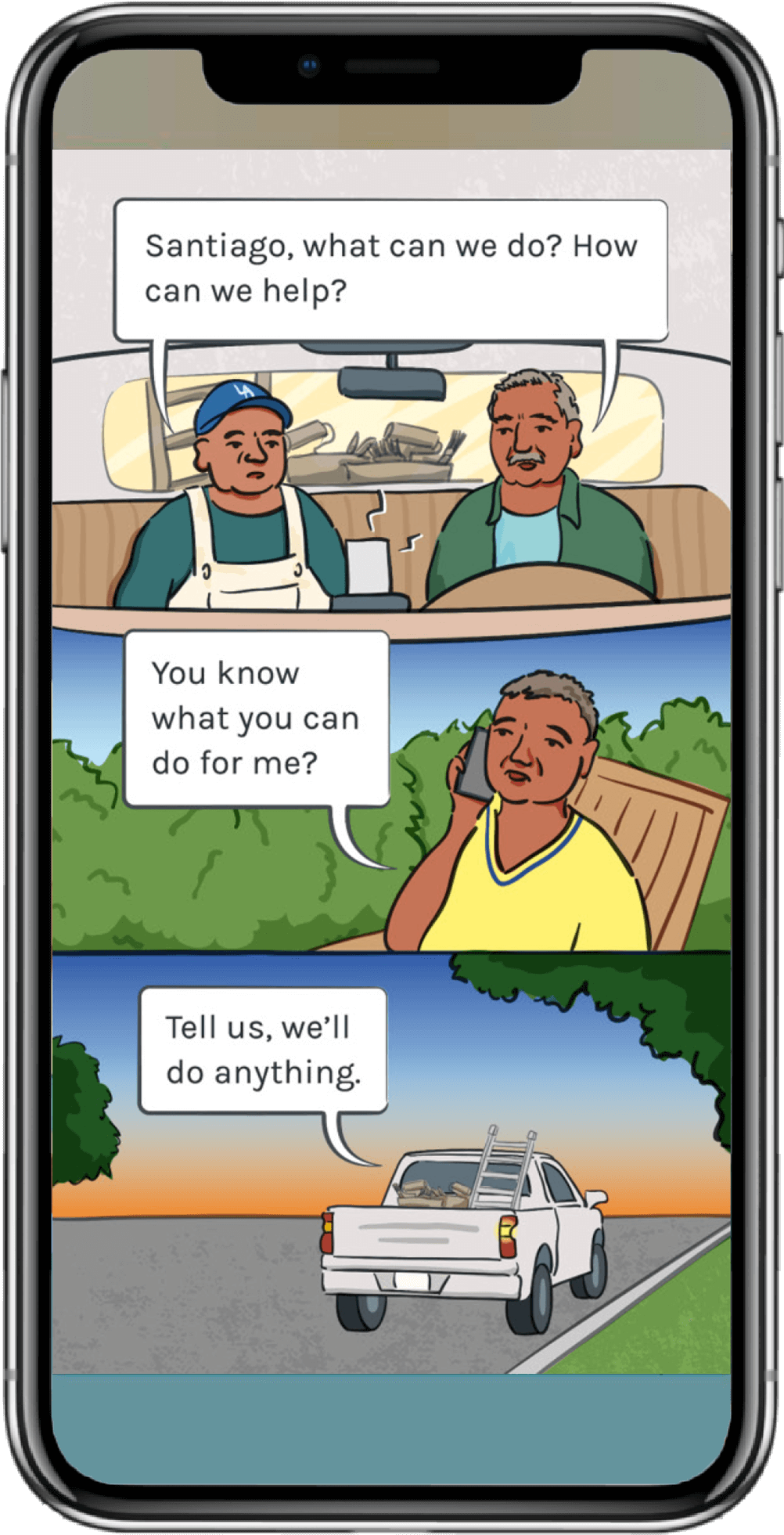
We all tend to perceive ourselves and our environment subjectively. When creating outreach and streaming content, organizations should strive to create characters and storylines that resonate with their audience.
For example, the fotonovela to the left used in a colorectal cancer screening program was developed in Spanish and English with separate versions for men and women. To ensure that the fotonovelas were compelling, the storyline used characters who were 50–75-year old Hispanic or Latino patients and who looked and talked like they could be the patient’s best friend or neighbor.
Cultural Humility
Cultural Humility is an ongoing process of self-exploration and self-critique combined with a willingness to learn from others. Listening and evolving are key parts of this process. Use technology to listen and collect back data to help you learn and adjust your programs at scale.
Want to learn more about use cases and opportunities around health equity? Digital Strategies to Support Health Equity serves as a compelling guide for organizations committed to dismantling the barriers to health equity through innovative digital solutions. It offers a glimpse into mPulse’s commitment to using technology to enhance accessibility, literacy, and personalization in healthcare, aiming to create a more equitable future for all.






