During the 2024 Open Enrollment Period, a record-breaking 21.3 million people chose “Affordable Care Act (ACA) Marketplace coverage according to the Biden-Harris Administration. The demand and need for this federal program are at an all-time high, as millions of Americans rely on access to this healthcare coverage.
While there have been continuous increases in enrollment year over year, many consumers are still facing challenges when signing up for marketplace coverage. Navigating through the process without support or tools to help guide them, individuals may not get the coverage they truly need for better care.
As an industry, it’s imperative to come together to uncover and address those challenges, so the millions of individuals relying on this coverage can navigate the enrollment process with ease.
The 2023 KFF Survey of Consumer Experiences with Health Insurance brought to light that individuals with Marketplace coverage were more likely to have challenges while shopping and enrolling in their health plan than those enrolled in other types of health coverage. They asked a series of questions about consumers’ experiences and identified the top challenges and barriers to enrollment.
Top 5 Causes of Consumer Confusion with Marketplace Enrollment
1: Option Overload & Finding a Plan That Meets Needs
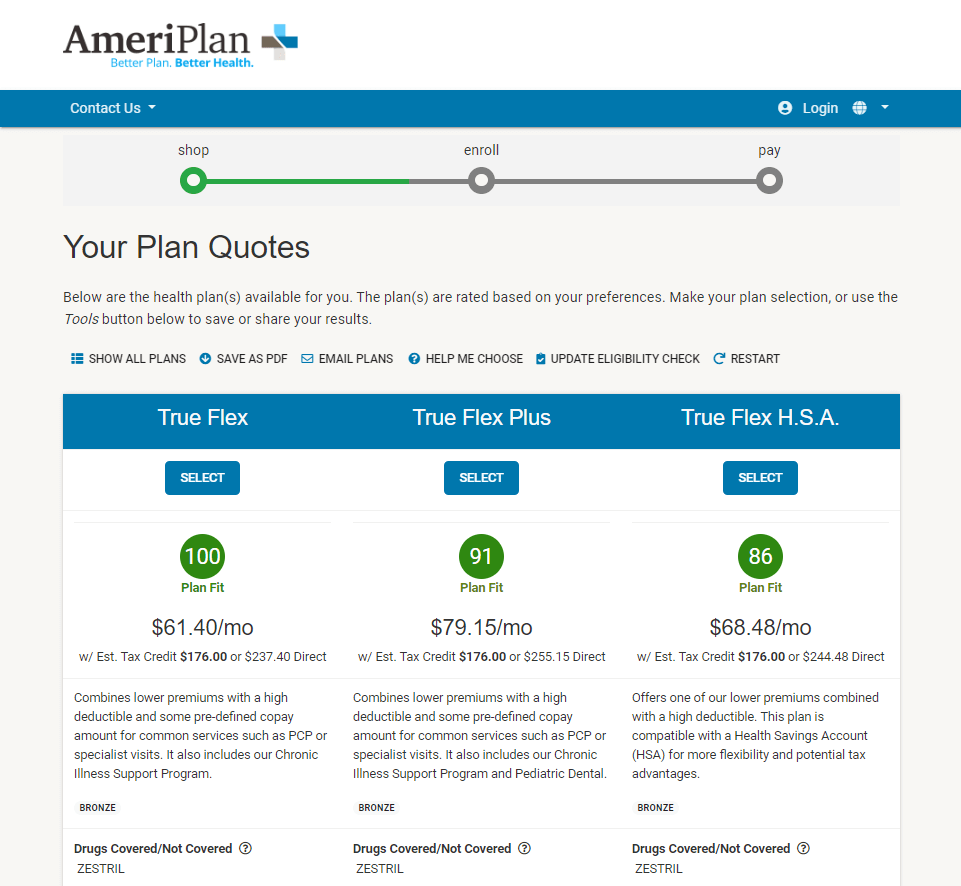
The average number of plans available to consumers on the Marketplace has increased from 25.9 in plan year 2019 to 113.7 in plan year 2023. With so many plan choices and the feeling of option overload running high, consumers are facing difficulties making a meaningful and informed selection when comparing plan offerings.
Consumer fatigue and frustration, confusion around plan offerings, and too many choices can cause individuals to feel overwhelmed and misinformed when shopping for an exchange plan. Without the proper tools in place to help guide consumers in their decision-making process, a lot can be left on the table.
Carriers offering exchange plans can help overcome this challenge and help consumers in a few ways. One is to work with an enrollment SaaS partner, like HealthTrio by mPulse, who offers an EDE Phase III integration. By doing this, they’ll be able to skip the healthcare.gov redirect and keep consumers shopping for exchange plans on their site throughout the entire enrollment process.
By reducing the high volume of plan options available from all carriers and only showcasing the plans they offer, consumers can easily navigate through and select a plan that best fits their unique needs.
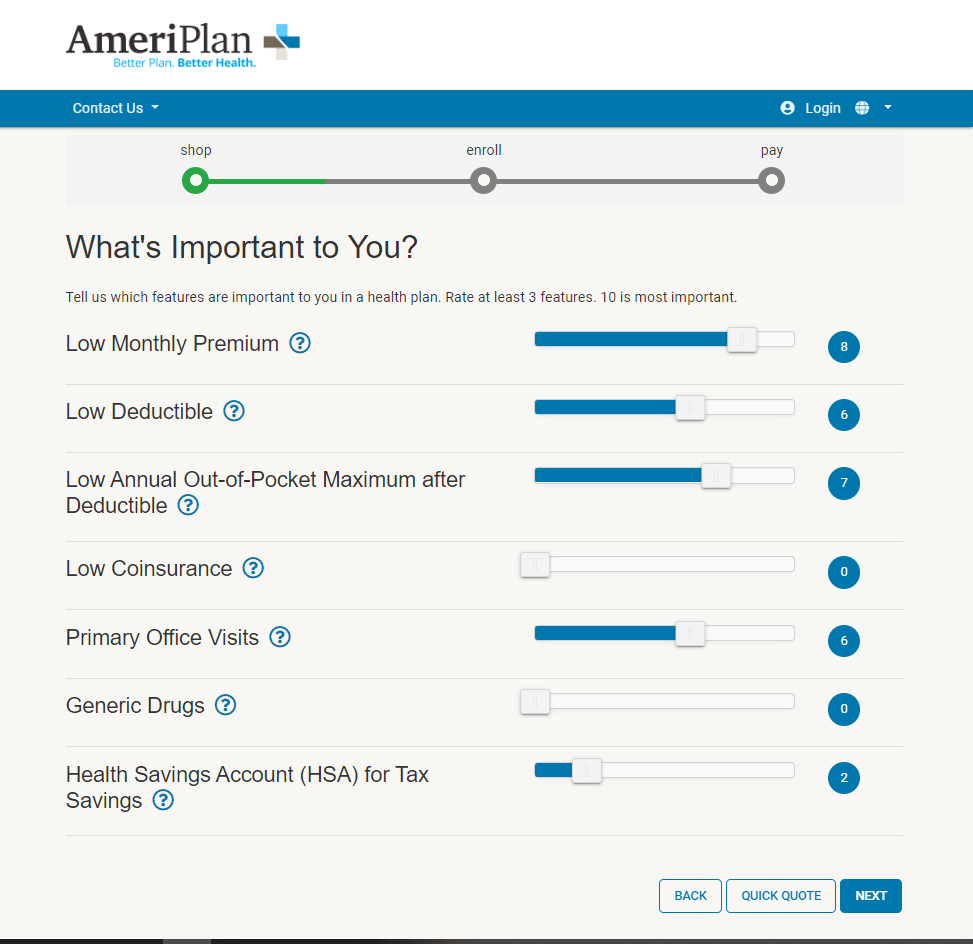
Another way is to implement plan shopping tools with built-in side-by-side plan comparison and decision-support.
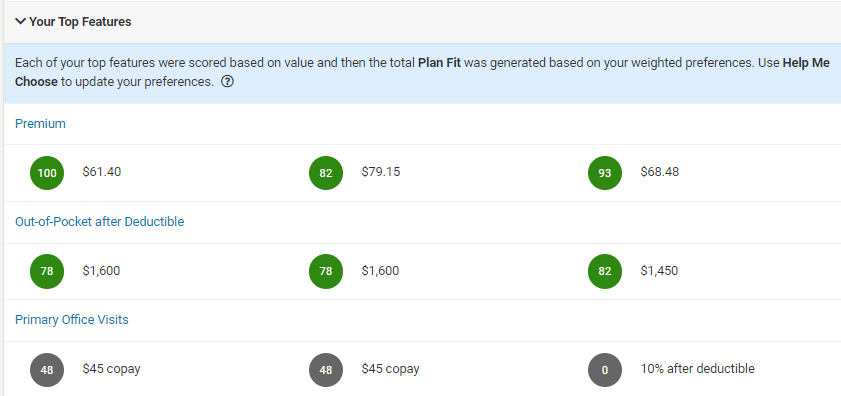
By asking consumers what is most important to them when selecting health coverage, using their answers to present plans that answer those needs, and comparing those plans based on specific elements like deductibles, premiums, and more, you can help them feel confident in their decisions and help them overcome barriers in the decision-making process.
2. Completing the Application or Enrollment Process
To many healthcare consumers, the application and enrollment process for health coverage can be a daunting task. Facing challenges such as complicated rules, tedious and lengthy forms, and industry-specific language can cause frustration and confusion to many individuals who are unfamiliar with the insurance industry.
With 32% of healthcare Marketplace enrollees saying they find basic health insurance terminology, such as “deductible,” “coinsurance,” and “allowed amount” difficult to understand, overcoming this challenge is critical to ensuring consumers feel educated enough to successfully shop and enroll in healthcare coverage.
Simplifying and streamlining the process will ease concerns and ensure a smooth path to enrollment. HealthTrio by mPulse does this by offering easy-to-understand and direct instructions, brief forms, a glossary of health insurance terminology used throughout the process, and user-friendly tabbed interfaces that will improve the consumer health plan experience and lead to increased membership for exchange health plans.
3. Understanding if Income Qualifies Them for Financial Assistance
Many consumers (9 in 10) who enroll in exchange plans qualify for and receive some form of financial assistance through premium tax credits and cost sharing reductions.
Even with roughly 90% of individuals qualifying, a common question and frustration when shopping for exchange plans is even understanding whether the person will qualify based on their income and financial situation.
As part of the eligibility and healthcare enrollment process, carriers can incorporate an easy-to-follow questionnaire to determine qualification for financial assistance.
By guiding the consumer through this process and taking the burden off them, carriers are ensuring those shopping for exchange plans understand all options available to them in order to make the best decisions for their current situation.
4 & 5. Difficulty Comparing Copays and Deductibles Under Plan Options / Hard to Compare Monthly Premiums.
The 2023 KFF Survey of Consumer Experiences with Health Insurance found that almost one in three adults found it difficult to compare two key elements, copays and deductibles, when shopping for a plan.
Similar to difficulties with comparing copays and deductibles under plan options, 25% of consumers found it difficult to compare monthly premiums of their plans of interest.
Ensuring people know how much they are expected to pay for their plans each month, what is financially required of them at each visit through copays, and knowing their plan deductibles helps to set them up for financial success.
Many individuals who qualify and enroll in healthcare exchange plans are from lower-income households where accounting for every dollar counts, so transparency into and understanding of their financial responsibility is a necessity.
During the shopping and healthcare enrollment process, health plans should ensure that their plan comparison tools include the ability to compare plans based on these specific line items. Doing so leads to transparency when it matters most and building trust with consumers long before health plan membership begins.
How HealthTrio by mPulse Can Help Health Plans Solve These Challenges
Knowing and understanding the top challenges and frustrations of consumers when shopping for and enrolling in Marketplace coverage is just the beginning.
Taking the steps to resolve these challenges and make the overall process easier is important to increasing plan membership, delivering a better consumer and member experience, and retaining members year over year.
HealthTrio by mPulse has been a trusted partner to leading health plans for over 20 years. By leveraging our purpose-built plan shopping and enrollment software, you will help alleviate the confusion consumers are currently facing when shopping for exchange plans, and help consumers overcome barriers to enrollment with specially designed tools.
We understand that most consumers are overwhelmed with picking a health insurance plan and have unique shopping needs, which is why our healthcare Enrollment product takes the pain out of the process and allows health plan consumers to make choices their way.
To learn more about our products and expertise, contact us.