But First, Who are SNPs?
A special needs plan (SNP) is a Medicare Advantage (MA) coordinated care plan (CCP) specifically designed to provide targeted care and limit enrollment to individuals with special needs.
There are three SNP categories:
- Dual Eligible SNP
- Chronic Condition SNP, and
- Institutional SNP
What is a D-SNP?
Dual Eligible Special Needs Plans (D-SNPs) enroll individuals who are entitled to both Medicare and medical assistance from a state plan under Medicaid.
The Dual Eligible Special Needs Plans (D-SNP) market continues to expand, with 851 plans offering coverage this year, a 112% increase from 2018. 12.5 million Americans have dual eligible status, but enrollment is only at 5.8 million, indicating further growth potential. Unlike their traditional Medicare Advantage counterparts, SNP members are provided with additional Special Election Periods (SEP), which allows them to switch plans outside of typical enrollment periods, heightening the need to deliver exceptional member experiences. With the Centers for Medicare and Medicaid Services (CMS) cracking down on look-alike plans, differentiation, acquisition, and retention have become top priorities.
Here are four strategies to consider in helping your plan retain D-SNP members
1. Provide a Seamless Onboarding Experience
Creating meaningful relationships with your members and establishing trust begins the moment a member enrolls in the plan. Welcoming new members to the plan ensures you get off to the right start and drives awareness around available benefits while ensuring members get established with in-network care and begin recognizing their plan as an integral part of their care team. Connecting with members early on also provides an opportunity to get to know your members better, allowing you to provide tailored and personalized experiences while uncovering valuable data insights at both the individual level, and a population level.
SNP members are typically offered supplemental benefits that Medicare doesn’t cover, such as dental, hearing, vision, food benefit cards, over-the-counter (OTC) benefits cards, transportation services, adult day and caregiver support, and more. Promoting awareness and utilization of available benefits as a part of the onboarding experience is critical as it increases the likelihood of utilization. Engaging with members at scale is challenging, particularly SNP members, who face greater barriers and accessibility hurdles. By leveraging an omnichannel approach to outreach to your members, you can begin to engage with them in the ways they prefer. mPulse offers an omnichannel combination of healthcare SMS messaging, email, IVR, mobile web, and print channels to engage members based on individual preferences. Engaging through multiple channels extends reach and allows members to interact with their plan across critical health topics while identifying and overcoming barriers at scale.
Applied Use Care: New Member Onboarding
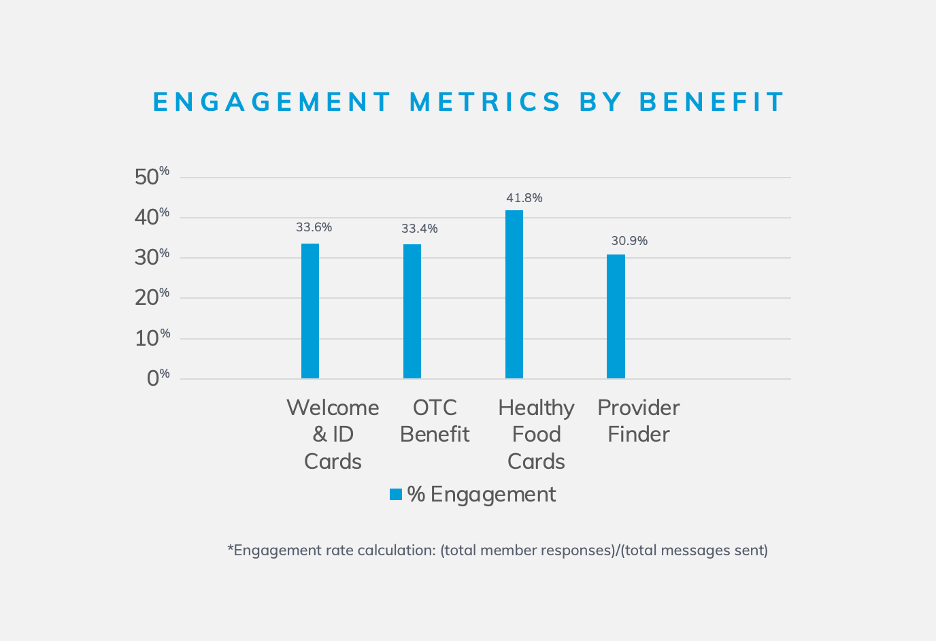
A leading national health plan partnered with mPulse to deliver SMS messages to new SNP members, welcoming them to the plan and driving awareness of related plan benefits and services.
During the 3-week onboarding program, members were delivered 4 SMS messages with in-message links and CTAs to plan benefits.
1st message: Welcomed members and confirmed receipt of their ID cards in the mail
2nd message: Promoted utilization of the OTC card benefit
3rd message: Promoted the utilization of a healthy food card benefit
4th message: Helped them find and select an in-network primary care provider.
Overall, the program saw a 99% reach rate and 58% engagement, with engagement being defined as opening a message and/or clicking a link. This program demonstrates increased awareness and utilization of plan benefits using healthcare SMS messaging to connect with DSNP members.
2. Make Healthcare Easy to Understand and Navigate
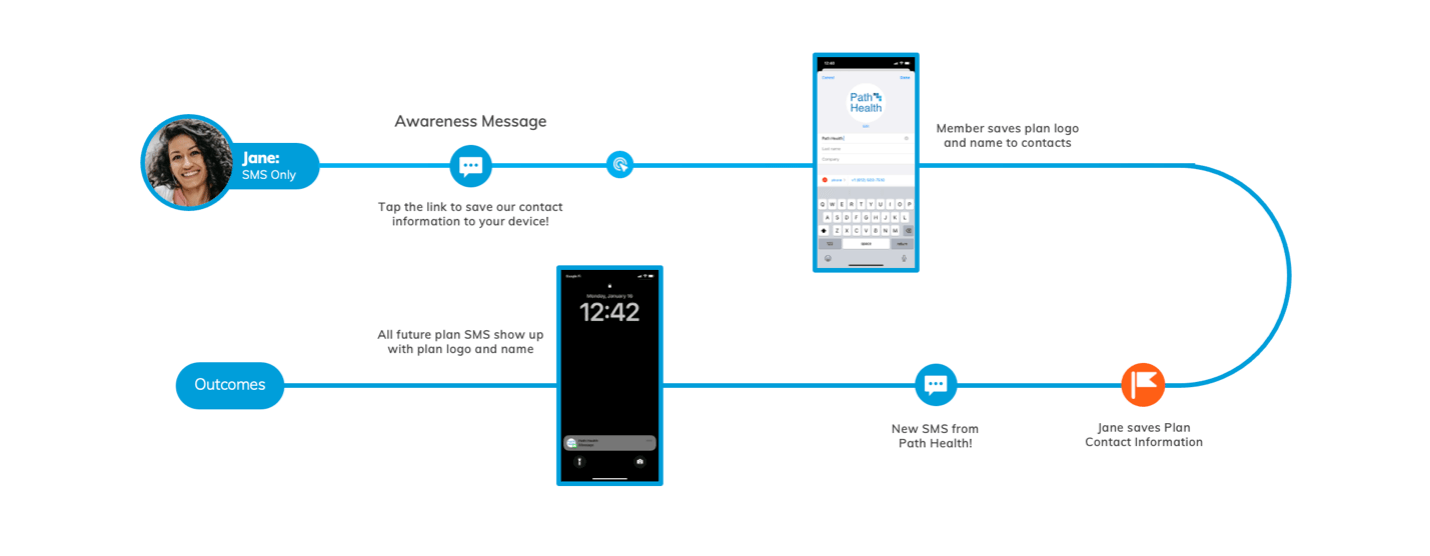
Healthcare is complicated, particularly for members managing one or more chronic conditions or who live with a disability. Making it simple for your SNP members to navigate their care will further build trust and lead to retention. One key way to build recognition digitally is using virtual contact file (VCF) cards. VCF card links can be sent via SMS, and your members can click a link that saves the plan phone number and contact information in their address book. This makes it easy for members to reach their plan and increases the likelihood they’ll answer an inbound phone call or SMS message.
mPulse typically sees approximately 30% of members clicking through to save their health plan’s contact information to their address book when a VCF card link is used and promoted within messaging.
Because SNP members are assigned case managers to help them navigate and coordinate care, seamless communication and relationship building with their assigned care manager is essential. mPulse offers seamless 1:1 healthcare SMS messaging with care managers and members via Engagement Console.
Engagement Console is a user-friendly tool that allows members to switch from automated SMS messages to live messaging with care managers through text-in keywords. This enables care managers to intervene and support at critical moments, further building trust and helping them see their plan as a reliable partner in their healthcare journey.
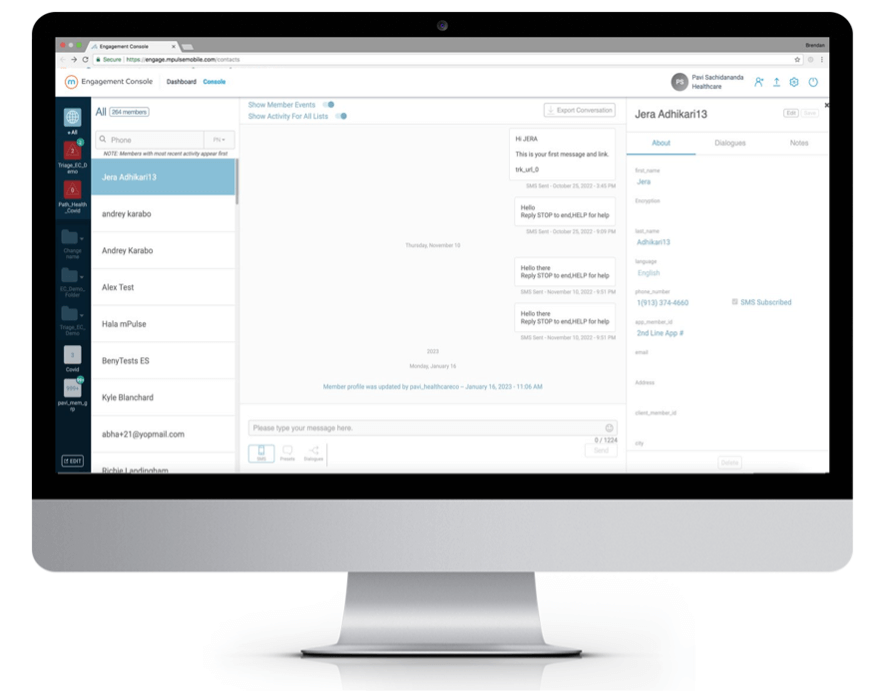
Applied Use Case: Engagement Console
A leading health plan operating in multiple states leveraged mPulse’s Engagement Console to improve member retention and increase CAHPS performance and member satisfaction. By switching from live call outreach to Engagement Console, the plan reached 2X more members and increased staff capacity by 3X.
3. Broaden Access to Deliver Equitable Care
With the Health Equity Index (HEI) accreditation reward factor announced by CMS for 2027, plans can be incentivized to reduce health disparities. The HEI is particularly critical among SNP populations, where opportunities to broaden access and provide additional support are most prevalent. To uncover barriers, plans must proactively identify and address members’ needs at key moments throughout their health journey.
Cadenced and timely touchpoints help members stay on top of their care. They enable proactive plans to empower members to adhere to their medications, schedule preventive care visits, and drive awareness around available resources and plan information.
mPulse’s ready-to-deploy programs leverage omnichannel outreach to proactively engage members across critical healthcare topics. Our messaging content leverages behavioral science techniques designed to empower members to take health action and includes healthcare-specific Natural Language Understanding (NLU) and conversational AI in 7+ languages to decipher a range of member responses throughout the program’s duration to deliver the right message at key moments to overcome barriers.
For example, if a member replies to a message telling us they don’t own a car or can’t drive, our NLU will recognize this as the member needing transportation and deliver a message with applicable plan-related CTAs to the member. Identifying and overcoming barriers at key moments helps improve accessibility and delivers a seamless experience at scale to increase satisfaction.
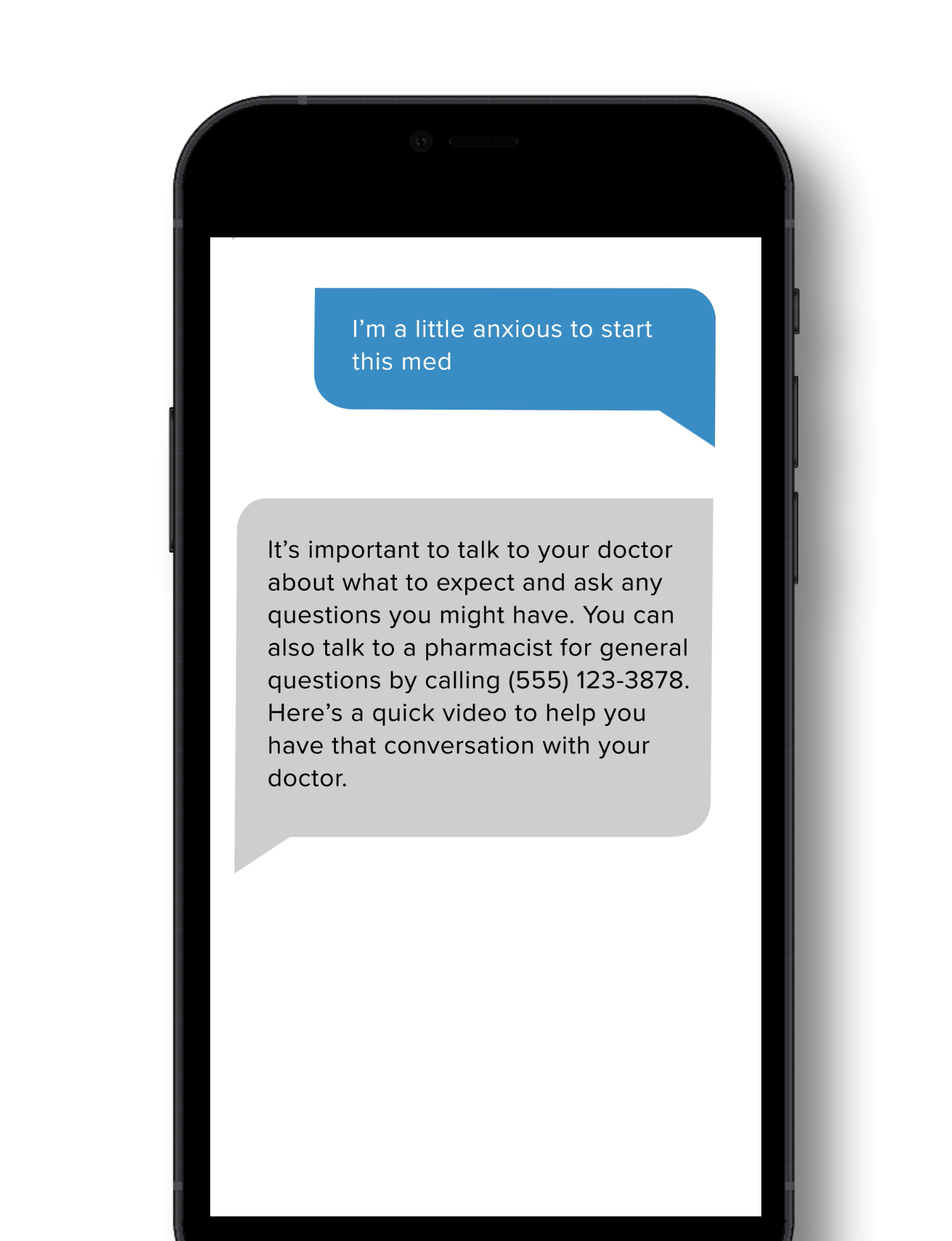
Applied Use Case: Medication Adherence
A leading health organization partnered with mPulse to improve medication refill rates among their D-SNP population to improve health outcomes and Part D triple-weighted Star measures. A combination of SMS, Email, and IVR outreach was used to send automated refill reminders for Diabetes, Hypertension, and Cholesterol medications. A barriers assessment was sent to members who were non-adherent and hadn’t engaged with reminder outreach messages. 41% of engaged members received the barriers assessment in which their barrier was identified, and they received relevant messaging and support in response.
Common barriers include issues with transportation, concerns about medication side effects, concerns about cost, and forgetting to fill. Additionally, mPulse sees approximately 20% of members requesting ongoing reminders to fill their medications.
By leveraging mPulse’s medication adherence program, the plan saw a 29.2% improvement in members filling their needed medications within 7 days of outreach compared to the control group. (The control group did not receive outreach.)
4. Continuously Optimize and Refine Your Approach
To retain SNP members, you need to understand what your beneficiaries need and want at both the individual and population levels. By aggregating and assessing a combination of internal and external data sets, you can gain valuable insights that enable your plan to be strategic and data-driven when making decisions that inform your retention strategy.
Decision Point Analytics uses over 90 predictive models to deliver highly accurate predictions at the population and member levels. Plans can leverage this data to be proactive around when and to whom they deliver outreach to ensure members get the right touchpoints and interventions at key moments, decreasing unnecessary outreach and ensuring members who require a higher touch receive timely engagement. Being able to triage outreach based on each member’s most pressing health challenges and issues allows members to feel valued, further building trust that leads to meaningful relationships over time.
Applied Use Case: CAHPS and Member Experience
A leading national health plan partnered with Decision Point Analytics to improve CAHPS performance and member satisfaction using predictive models to assess which members were most to least likely to respond negatively across key CAHPS performance measure areas: Plan Satisfaction, Drug Plan Satisfaction, Access, and Provider Satisfaction. Members flagged as high risk for responding negatively were contacted directly by a plan representative to assess and address their needs. Members identified as least likely to respond negatively were sent outreach to ensure the relationship remained positive.
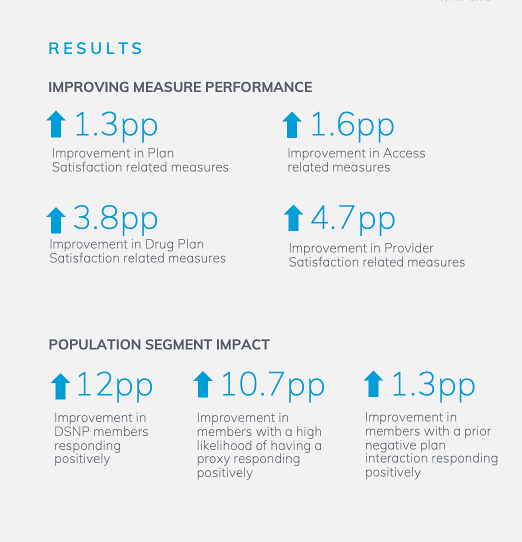
Across CAHPS-related measure areas, the plan saw a
- 1.3 percentage point improvement in plan satisfaction
- 1.6 percentage point increase in access
- 3.8 percentage point improvement in drug plan satisfaction
- 4.7 percentage point improvement in provider satisfaction.
- For segment impact, the plan saw a 12 percentage point improvement in D-SNP members responding positively.
In Summary
D-SNP members are an incredibly diverse group that faces greater barriers to healthcare and is notoriously hard to reach. Due to their complex needs, SNP members require a higher-touch approach, presenting plans with an opportunity to reduce health disparities and provide exceptional care experience that leads to improved health outcomes and meaningful relationships.
To improve quality performance and retain their most vulnerable members, plans need to address and assess individual needs using powerful digital solutions to identify and overcome barriers and provide tailored experiences. A combination of internal and external data sets and experiential insights enable plans to be data-driven and strategic in their approach to retaining D-SNP members.






