Medicaid is a vital safety net for millions of low-income and vulnerable individuals across the U.S. However, glaring health disparities persist within the program.
The pandemic underscored the stark health inequities among marginalized communities, including BIPOC (Black, Indigenous and People of Color), LGBTQIA+, people who are neurodivergent, and people with differing physical abilities. These challenges are especially pertinent to Medicaid, since more than half of Medicaid enrollees are people of color, and an estimated 20 percent are considered disabled.
Although tackling health inequities is a massive, multi-stakeholder undertaking, innovative solutions and strategic changes can have a significant impact, especially in the realm of digital health technology.
Digital health tools play a crucial role in eliminating health inequities and improving care for all. But technology alone isn’t the answer. Investing in technology without a clear strategy to advance equity can actually exacerbate existing inequities. Instead, health organizations need to address health equity by combining data-driven practices with a whole-person approach that grounds services in humanity and ensures all people receive the care they deserve.
Why Medicaid has Vast Health Disparities
Health organizations are undergoing a reckoning about the ways the insurers, providers and the greater healthcare community have failed marginalized communities. Tangible steps must be taken to fix systemic problems.
That includes viewing health from the whole-person perspective. It’s estimated that about 80 percent to 90 percent of health outcomes can be attributed to social determinants of health (SDOH) – non-medical factors such as socioeconomic conditions, environmental factors, race, ethnicity, language, sexual orientation and gender identification (SoGI).
It can be all too easy for providers to make assumptions. For example, some providers may write off a Latino patient as non-compliant when they don’t take prescribed medicines without further investigation or may ignore a female patient’s pain because it was seen as common period symptoms. However, a Latino patient may not take medication because it’s cost-prohibitive or they don’t have a pharmacy near them, while the other patient’s pain could be a symptom of a more serious illness that requires medical intervention.
If a provider has more time to connect with patients, listen to their perspectives and treat them as individuals, they can better identify their needs and identify solutions, such as prescribing a lower-cost formulary or scheduling a follow-up appointment with a specialist.
While these SDOH-related health disparities exist for all individuals, Medicaid members face another unique hurdle that affects their healthcare experiences – stigma and negative stereotypes about their use of government services. Although individuals must meet stringent criteria to qualify for Medicaid, organizations and even providers themselves may perpetuate stereotypes about people who need government services — increasing barriers to care rather than eliminating them.
It doesn’t help that there are significant data gaps among Medicaid populations that hinder organizations from understanding and addressing the myriad factors impacting people’s health outcomes and access. Approximately one in five Medicaid beneficiaries are missing information related to their race and ethnicity. These gaps make it even more challenging to pinpoint and prioritize areas for health equity initiatives.
So, with all of this in mind, what can health organizations do to address these complex challenges and bridge the health equity gap? Advancements and innovations in digital technology create new opportunities for health organizations to identify and track health disparities, and target services and medical interventions for vulnerable populations.
But to make progress on health equity goals, organizations need strategies and structures that put people at the center of the health care experience.
3 Ways to Reduce Health Barriers
While digital tools and data-driven strategies can streamline processes, reduce friction and enhance consumer experience and engagement, effectively using these tools to serve and support vulnerable populations poses a unique challenge.
The following considerations can help organizations focus their technology strategy to better support those who are most in need.
Focus on establishing trust.
Trust is often the determining factor when it comes to a patient refilling their prescription, showing up to a follow-up appointment or making a healthy change in their behavior. But establishing trust among Medicaid beneficiaries can be even more challenging in light of the historical medical discrimination and mistreatment of marginalized populations, as well as government recipients’ current experiences with medical bias.
Building trust requires empathy, transparency, and an in-depth understanding of individuals and their unique needs. Robust data analytics can help with this. By collecting and analyzing data on race, ethnicity, language, sexual orientation and gender identity, healthcare organizations gain actionable insights that can help identify disparities and tailor interventions to meet the unique needs of diverse populations.
With a better understanding of these needs, organizations can treat Medicaid beneficiaries as individuals and begin to rebuild the critical link of trust with their beneficiaries.
Meet people where they are.
Another way health organizations can increase access to care is by providing beneficiaries with meaningful interactions and tailored personalized engagement. In fact, nearly two-thirds of consumers would access additional care if their healthcare experiences were more personalized.
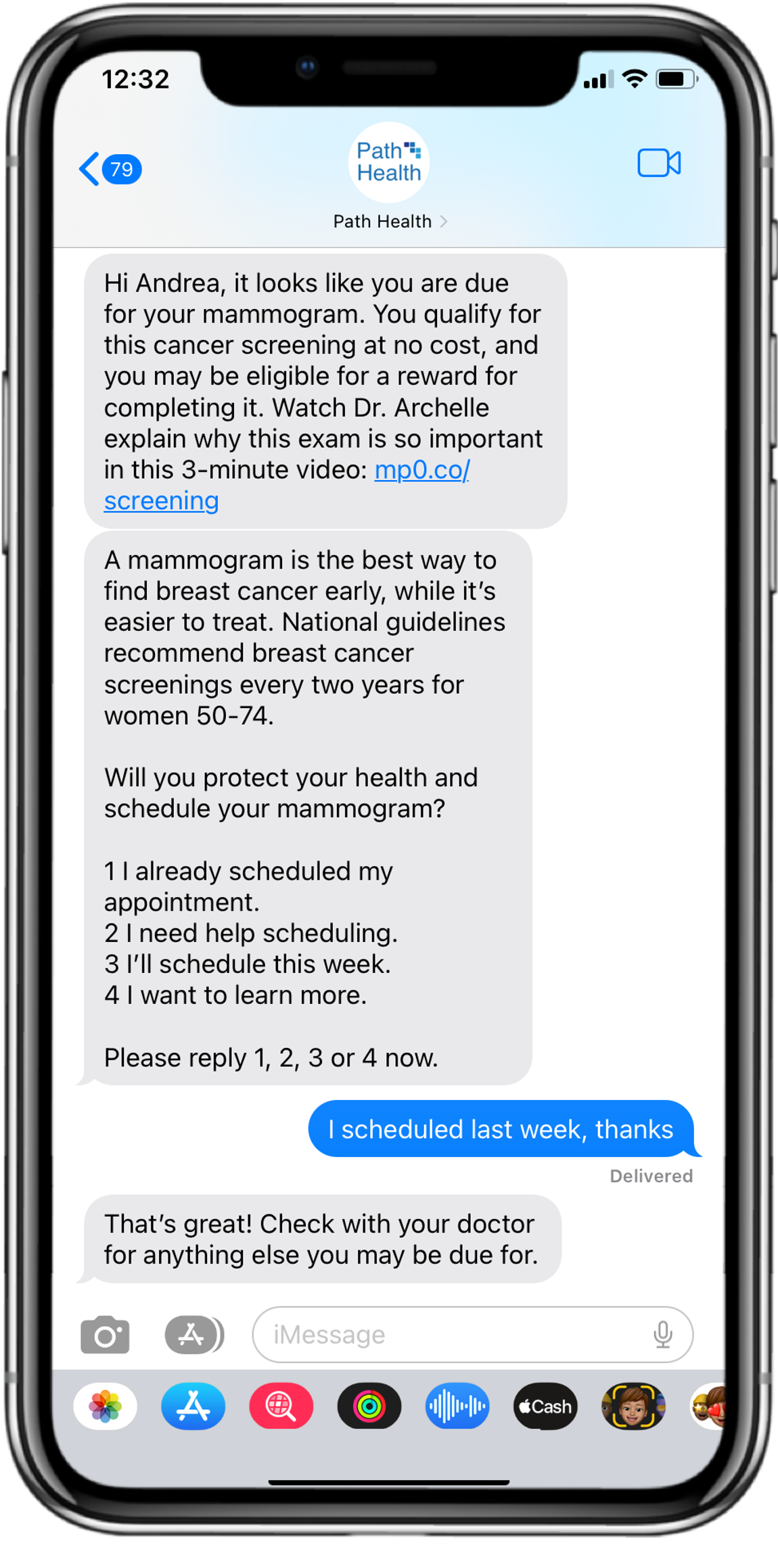
In particular, health plans should focus on improving accessibility to healthcare information and communicating with Medicaid members on channels they already know and use. For 85 percent of Americans, that’s on their smartphones. Digital health programs that use text messaging and other mobile channels can deliver personalized health information, reminders and resources to individuals in a convenient setting.
Programs like the national Affordable Connectivity Program (ACP) are helping close the digital divide (the inequitable access to computing devices and stable high-speed Internet) that can alienate Medicaid recipients, especially in rural communities.
Texting and other mobile technologies can not only provide timely updates and appointment reminders; they can also offer valuable educational materials. For example, health plans and providers can inform members of the importance of mammograms while removing common fears or provide members with limited literacy skills with high-quality videos that utilize best practices in learning strategy. By meeting beneficiaries on their terms (without condescension or stigmatization), health organizations can remove points of friction and make services more accessible.
Build for scalability.
It’s not enough to build digital experiences that only work in a single scenario or specific moment. Health organizations need to build processes that scale across operations and alongside organizations as they continue to grow. Artificial intelligence and automation are valuable tools to help organizations achieve these goals.
Administrative costs comprise a majority of health system waste, with at least half of administrative spending deemed wasteful. Automating manual tasks and supercharging data-driven decisions enables organizations to streamline burdensome administrative processes and enhance the overall efficiency of healthcare delivery at scale, ultimately improving care for patients.
While artificial intelligence technologies have vast potential to improve healthcare delivery, it’s crucial to ensure AI tools are used responsibly and avoid perpetuating existing disparities or biases in data sources. To minimize the potential negative effects of AI, set rigorous safeguards and standards that adhere to best practices established by trusted entities, like the Coalition for Health AI.
The Imperative for Digital Innovation
“Healthcare as usual” isn’t optimal for Medicaid enrollees, health organizations or anyone for that matter.
Programs that fail to address underlying disparities lead to greater inefficiencies and higher costs for organizations. In fact, treatment of chronic conditions such as asthma, cancer, diabetes and heart disease costs the U.S. $320 billion a year resulting from health inequities — and unaddressed health disparities costs could balloon to $1 trillion by 2040.
Technology adopted in a vacuum won’t solve deep-seated health disparities. But by pairing digital investments with meaningful conversations and support for Medicaid beneficiaries, we can begin to break down barriers and accelerate progress toward a more equitable healthcare system for all.
This article was originally published on healthdatamanagement.com on December 20, 2023.






