In the ever-evolving landscape of healthcare, digital engagement has become a cornerstone of member experience. As organizations strive to create seamless and personalized interactions, the role of member portals has expanded far beyond simple information hubs.
In our recent webinar, The Future of Portals: Creating Outcome-Driven Experiences, industry experts explored current trends driving the member portal space and how healthcare organizations can leverage engagement beyond just the portal itself to simplify the member experience, drive better outcomes, and stay ahead of the curve.
The Evolution of the Member Portal Experience
Traditional health portals have long been used to provide access to member IDs, claims history, and provider search tools. However, these static, transactional platforms are falling behind in meeting the growing expectations of today’s digitally savvy health consumers and the ever-changing regulatory requirements from CMS and state authorities.
Want the full details on The Future of Health Portals? Watch the on-demand webinar.
The new member portal experience is shifting to be more dynamic across the member experience and personalized based on user behavior, communication preferences, and real-time data. By embracing these new strategies, plans can anticipate consumer and member needs and proactively deliver a unified experience with relevant content and conversations across multiple channels, including plan enrollment, the member portal, SMS, and other preferred communication channels. Let’s take a look at how.
Jessica’s Journey: A New Standard for Digital Healthcare Engagement
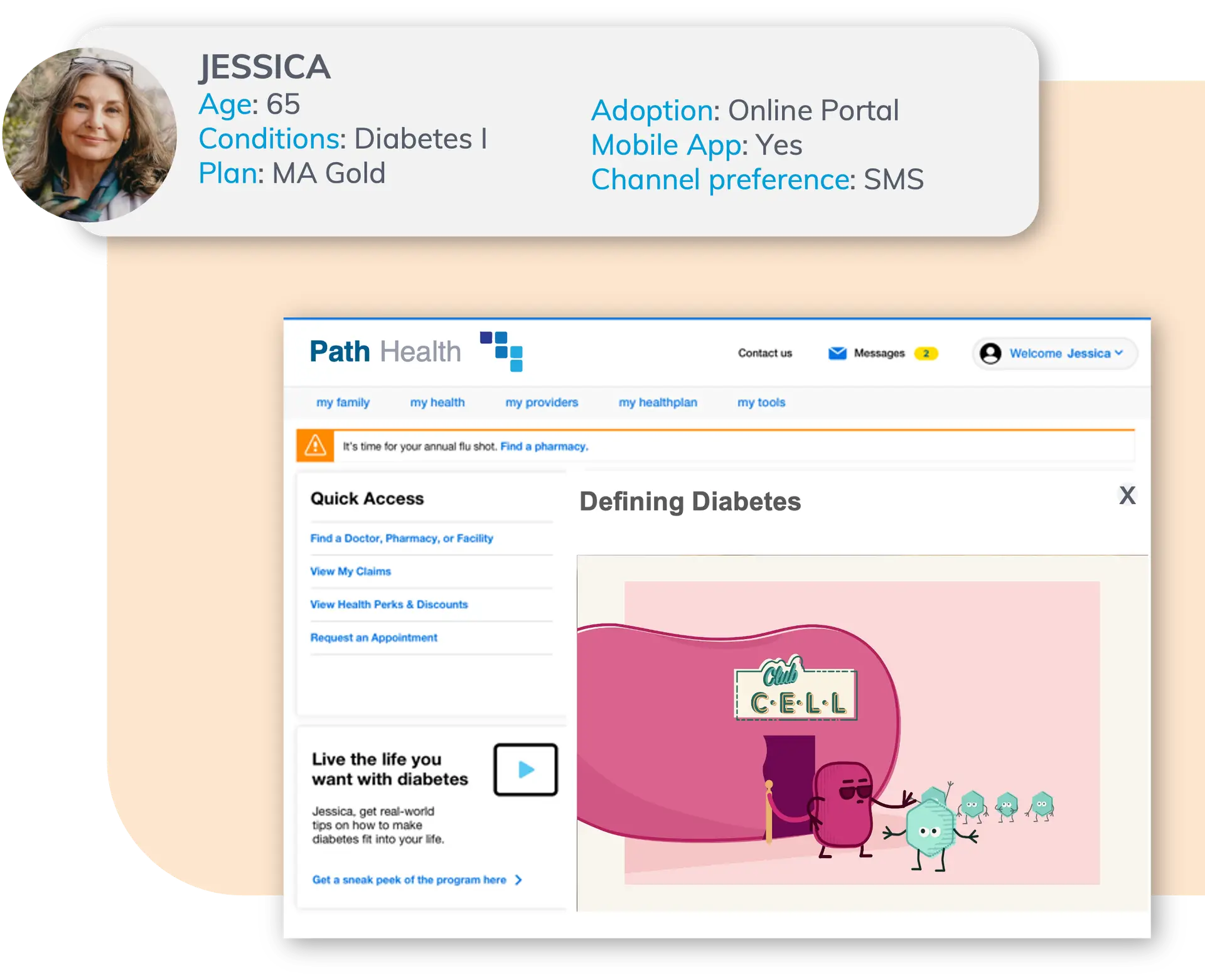
To illustrate this new health experience, let’s follow Jessica, a 65-year-old woman who just enrolled in a Medicare Advantage plan.
In the image below, you can see a typical journey for her when there is a lack of orchestration and personalization. It’s overwhelming and slightly chaotic, with each team focused on their own objectives: marketing sending out welcome messages, quality trying to communicate about upcoming surveys and open gaps in care, and so on. Different efforts, different point solutions. The result is an experience focused on the plan’s needs instead of on the member’s needs.
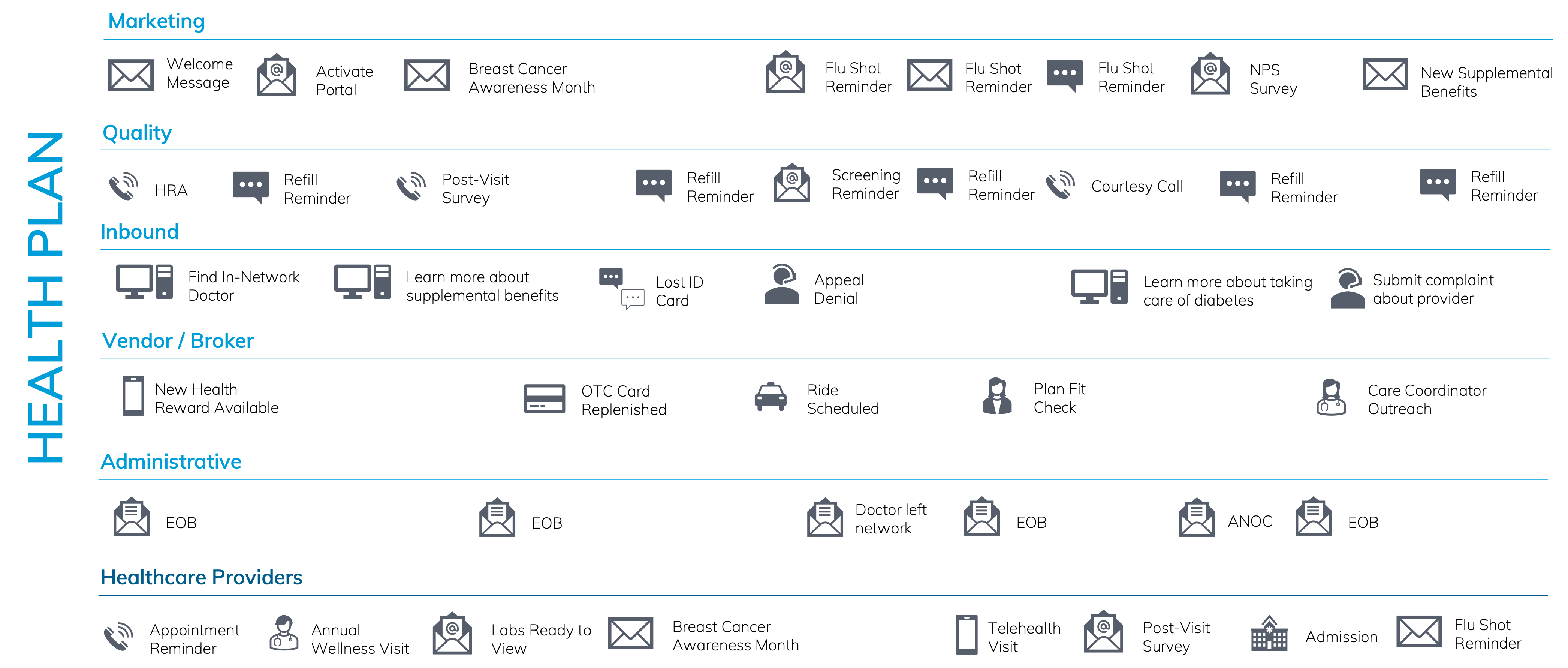
With an integrated experience, you have technology that can understand each member’s needs, preferences, enrollment, and disposition on certain channels and can orchestrate the journey so that it is centered around the member with all of the communication happening in harmony with each other.
The result is Jessica’s new journey.
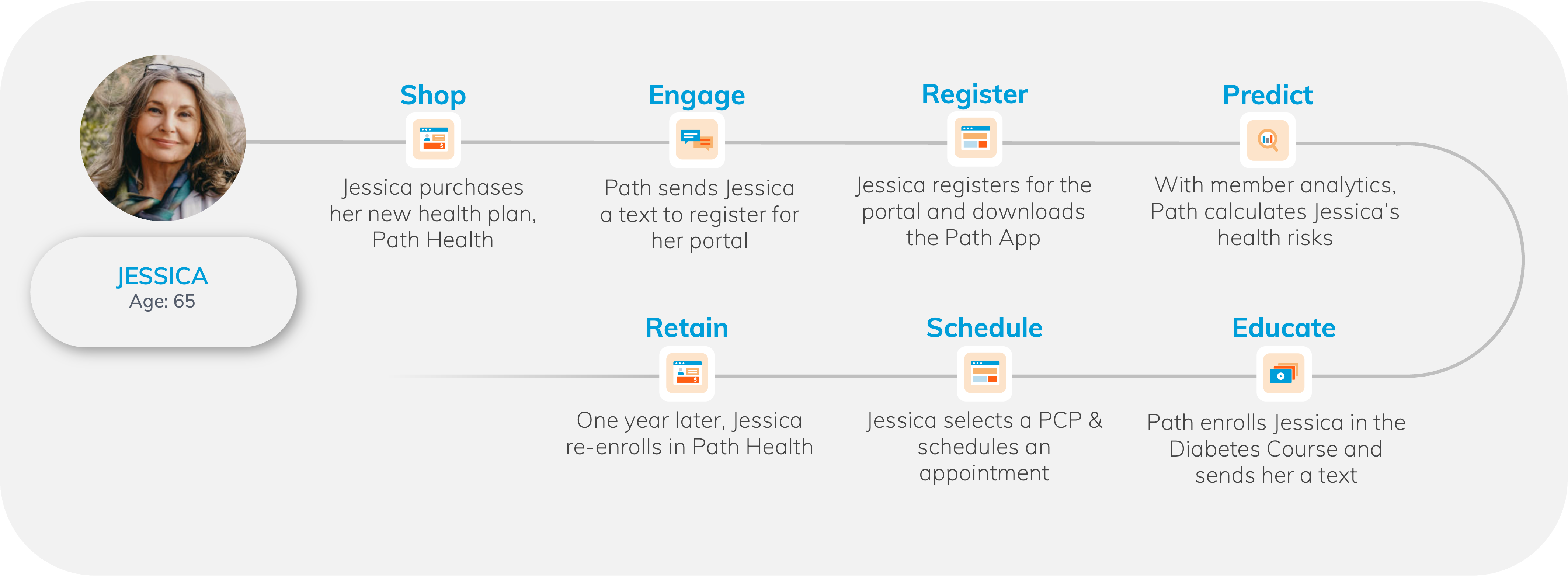
When she enrolls, her plan sends her a text that welcomes her and encourages her to register for her member portal, briefly highlights the key benefits and tools of the member portal, and provides a link to register for an online account, creating a seamless experience across channels.
Once registered and using the portal, the plan calculates Jessica’s health risks based on her current risk scores, claims history, and demographic information. Based on that calculated risk, the health plan proactively enrolls Jessica in a diabetic education course and texts her personalized education around treating her condition.
To streamline her experience, Jessica can log into her member portal to search for local providers and find information about service options along with their potential costs. Prior to scheduling her visit with a provider, she can find her Insurance ID Card and review her benefits and eligibility to ensure there won’t be any surprises during her appointment.
As the year progresses, the plan recommends Jessica renew her plan during the enrollment period. This is based on her lowered risk scores, her consistent utilization of the portal, and her responses to surveys and questionnaires available within the portal or through any of the outbound communications.
The various touch points that Jessica will have on her healthcare journey offer the health plan opportunities to gather and collect more information and insights about her conditions, preferences, and utilization. Those insights continue to update the information we have on her throughout the various touch points along her journey.
Jessica’s experience exemplifies the future of digital healthcare and the role of member portals within it—where engagement is proactive, personalized, and frictionless and modern portals empower individuals to take charge of their health with greater ease and confidence.
Three Key Trends for Member Portals
1. The Increasing Demand of Regulatory Compliance and Consumer Expectations
Health plans are facing increasing demands to adapt to a rapidly changing healthcare landscape, driven by new regulations and evolving member expectations. CMS and state agencies have introduced mandates requiring health plans to collect, store, and protect more comprehensive health data, facilitating secure data exchange among providers, members, and other health plans, and initiatives like the California Data Exchange Framework highlight the push for greater interoperability.
At the same time, members expect seamless digital experiences that offer convenience, such as easy access to health records, provider search, and direct communication with their care team. To remain competitive, health plans must invest in digital platforms that meet both regulatory requirements and members’ increasing expectations.
"For the first time, members reported a health plan's digital capabilities were more important to them than physician availability when considering switching plans."
Source: Voice of the Member 2023 Cognizant Tweet
By leveraging advanced data management and interoperable technologies, health plans can enhance care coordination, improve operational efficiencies, and impact health outcomes. For example, electronic prior authorization systems can significantly reduce delays in patient careby integrating seamlessly with providers’ electronic health records. Additionally, member-centric digital tools, such as portals, promote proactive health management, increasing member engagement, satisfaction, and loyalty. By embracing these innovations, health plans can transform regulatory challenges into opportunities for growth and improved healthcare delivery.
2. The Growing Impact of Personalization on Member Trust
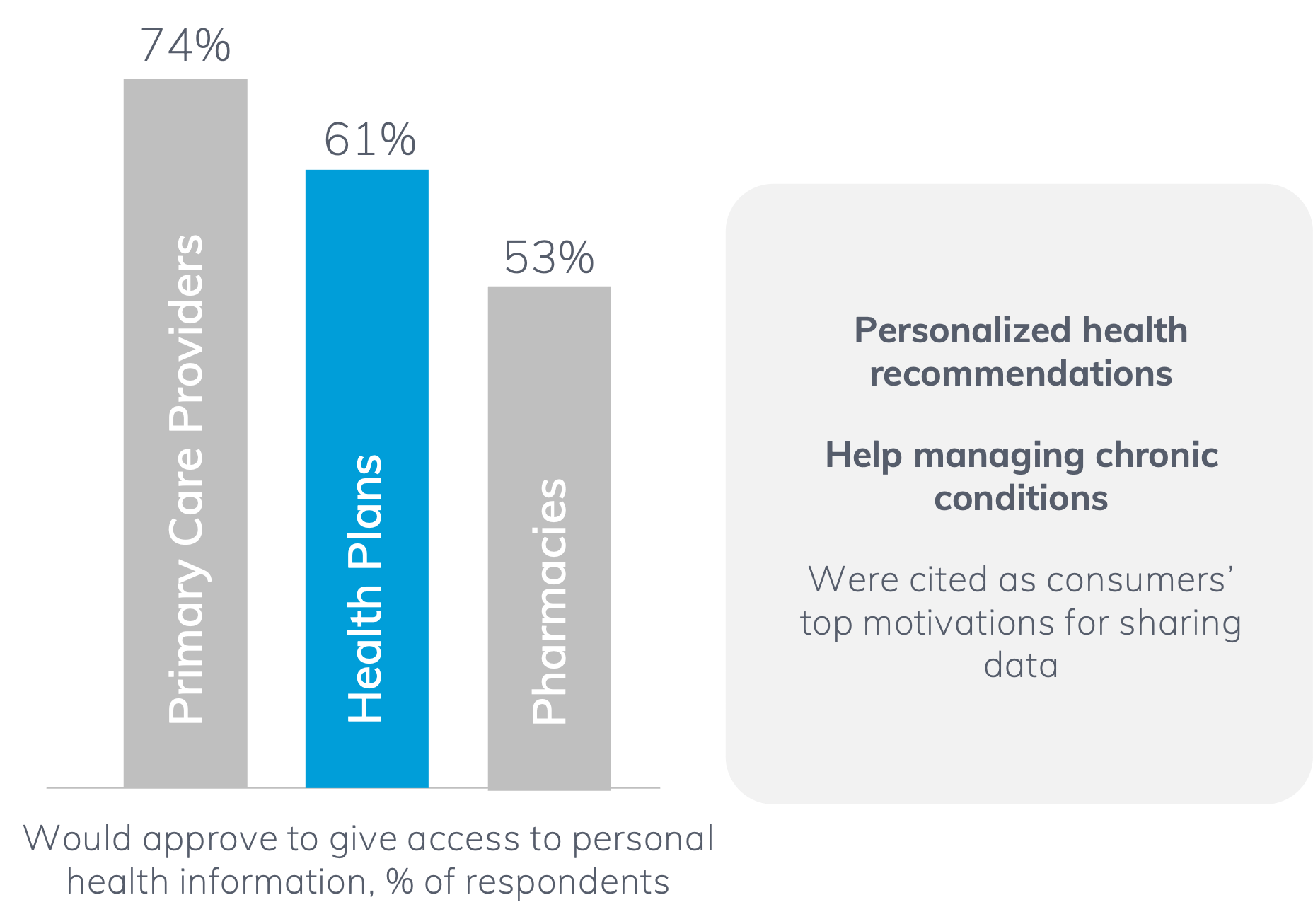 It’s clear: the future of member trust lies in personalization. According to a recent McKinsey survey, consumers are willing to trust organizations with their data—provided that data is used to improve their health. What is the best thing for a member to do at a given point to manage their chronic condition? What does the member need to know about their condition? What do they need to know about the medications they’re taking, and the treatment options they have?
It’s clear: the future of member trust lies in personalization. According to a recent McKinsey survey, consumers are willing to trust organizations with their data—provided that data is used to improve their health. What is the best thing for a member to do at a given point to manage their chronic condition? What does the member need to know about their condition? What do they need to know about the medications they’re taking, and the treatment options they have?
 A member portal provides a large playing field for that kind of personalized health experience for members. It starts with a foundation of flexible technology to deliver a relevant and accessible experience based on the member‘s eligibility data, their diagnoses, their demographics, their preferences, and the health plan products they’ve purchased.
A member portal provides a large playing field for that kind of personalized health experience for members. It starts with a foundation of flexible technology to deliver a relevant and accessible experience based on the member‘s eligibility data, their diagnoses, their demographics, their preferences, and the health plan products they’ve purchased.
On top of that, when you layer the security and privacy a portal affords, we can build trust with that member, ensuring that they have safe access to timely information, relevant content, and actionable tools. With that access, there is self-service enablement within the portal, encouraging task completion, acknowledging alerts or notifications, and prioritized interaction with recommendations that ultimately help the member in guiding their care.
3. Deployment of Powerful Omnichannel Engagement to Promote Portal Adoption
Omnichannel engagement has long been a key factor in relationship building with members, but it can also play a key role for portals.
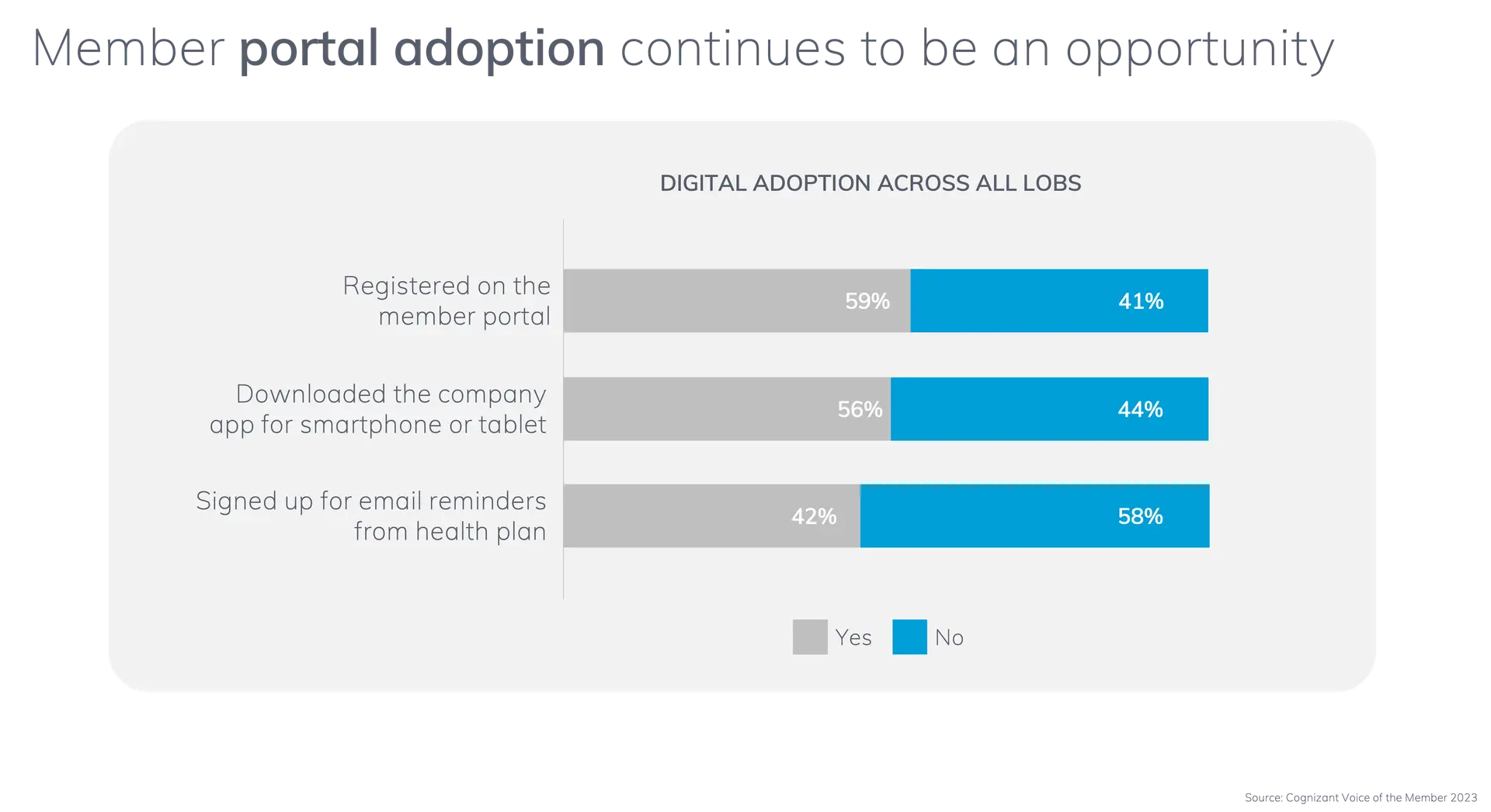 Though we know health portals can be a powerful tool for connecting the member, health plan, and provider, currently only 59% of members across all segments are adopting portals. So, how do we combine the benefits of digital engagement with the resource-rich portals?
Though we know health portals can be a powerful tool for connecting the member, health plan, and provider, currently only 59% of members across all segments are adopting portals. So, how do we combine the benefits of digital engagement with the resource-rich portals?
Start by making it easy for your members to access and adopt your health portal. Based on your member’s profile and journey, you can provide motivational and educational content around portal features that members can easily use, including finding a provider, getting updates on claims, paying premiums, or interacting with relevant health education content.
And most important, be where your members are. Where are most people? Whether bad or good, we are attached to our phones. So, meeting your members where they are means sending all that information directly to their phone where they’re most likely to see and engage with it. We know upwards of 97% of text messages are opened within the first three minutes (GET LINK). Delivery through this channel removes the largest barrier we face¾getting your members’ attention.
And what you send matters. mPulse’s recipe for effective health communication has a few main ingredients:
- Personalized behavior change techniques
Utilizing over a dozen techniques to overcome barriers in health equity and literacy while gaining trust to drive change - Centering the member for improved outcomes
Creating tailored programs that speak to the member’s unique needs instead of one-size-fits-all - Leveraging AI for more natural conversations
Conversational AI and Natural Language Processing create a better, less abrasive member experience to overcome barriers
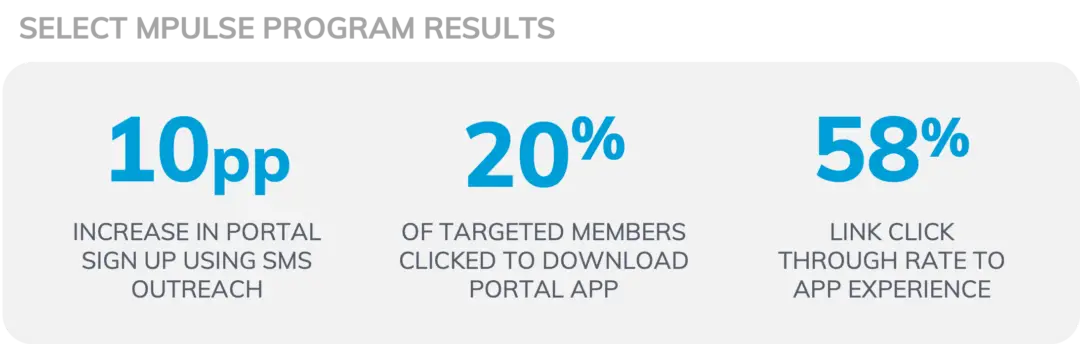
When plans have worked with us to deploy this kind of communication, they’ve seen impressive results: a 10 percentage point increase in portal adoption, 20% of targeted members clicking to download the portal app, and a 58% link click rate through to the app experience.
The Competitive Advantage of an Integrated HXI Portal
An integrated, consumer-centered experience is always the ultimate goal, and getting there is not so far off into the future¾it’s closer than we think. By personalizing the member experience based on their individual member-level data, delivering the communications necessary to engage them and promote adoption, and providing a secure, seamless navigation experience once they get there is well within reach.
Portals are no longer static repositories of information. They are dynamic, intelligent platforms that drive engagement and improve health and operational outcomes. As healthcare organizations evolve, embracing new technologies will be key to meeting the expectations of modern consumers and delivering a truly connected, personalized experience.
The future of portals is here—are you ready to transform your digital engagement strategy? Visit mpulse.com to learn more about our offerings.

The Future of Health Portals: Creating Outcome-Driven Experiences
Watch this on-demand webinar to hear about proactive strategies to boost portal adoption and how health plan portals are transforming through automation, integrations, and personalization.