By the time the end of March rolls around, we will have seen just over 1,100 days of continuous Medicaid and CHIP enrollment. Federal guidance within the 2023 Consolidated Appropriations Act effectively decoupled continuous enrollment provisions from the Public Health Emergency (PHE) and will allow states to resume their redetermination process as soon as April 1st.
Most states and many plans have already completed the first phase of the unwinding by encouraging enrollees to update their contact information to ensure they receive their renewal paperwork when it arrives in the mail. And while most all of us reading this piece are well aware of where we’ve been over the last year and what the next one might look like, a recent Urban Institute study in December 2022 found 6 in 10 adults in Medicaid-enrolled families were not aware of an upcoming return to the regular Medicaid renewal process.
You’re probably thinking, “How is this possible? It’s all we’ve been talking about and planning for months and months!” Well, maybe we shouldn’t be so surprised. Medicaid/CHIP enrollment increased by 20 million individuals since February 2020 accounting for nearly 30% of all covered lives. That’s 20 million individuals who likely have never completed a traditional or pre-pandemic redetermination and three years since the last time everyone else has. Lest we forget a lot has changed and occurred over the last three years in general.
Stats and surprises aside, we still have a long road ahead of us and a lot of work to do. Thankfully our regulatory friends like CMS and the FCC have stepped up to help keep individuals from slipping through the cracks. CMS has provided a strategic toolkit calling for states and plans to work together in timely sharing of enrollment data and contact information, for states to expedite content approvals or provide pre-approved language for member outreach, and for enhanced processes for moving individuals who no longer qualify for state-based programs to marketplace offerings. The FCC’s recent declaratory ruling that clearly states the provision of a phone number on an enrollment form constitutes as express consent allowing federal and state agencies and their partners to make Medicaid enrollment calls and send text messages without violating call or text prohibitions. Plans should take full advantage of the resources provided to them by incorporating each toolkit and clarified regulation into their overall member engagement strategy.
Key Engagement Factors for the Return of Redetermination
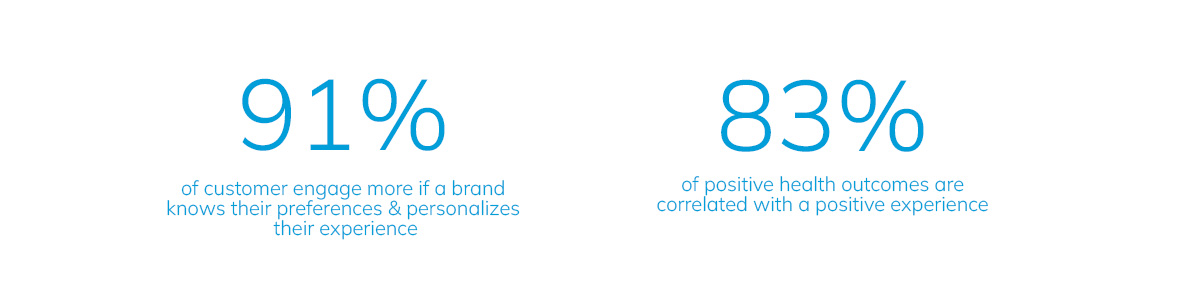
Now let’s talk engagement strategy. Most plans will be using CMS or state-approved content and timelines are tight, so there may not be as much room for the creativity we see when dealing with other engagement topics like closing gaps in care or encouraging timely rx refills. That doesn’t mean, however, that you can’t still take a strategic approach in areas where you can still have an impact, such as channels, personalization, and branding.
Channels: We know one single communication channel isn’t going to be enough, and it’s just not how people are consuming information or connecting to resources. Adult Medicaid beneficiary smartphone or tablet ownership rates are similar to the general US adult population, and 47.4% of dually eligible Medicare beneficiaries report using the internet to get information. An effective and successful engagement strategy is delivered through multiple channels by combining digital outreach like SMS and email with traditional modes of communication like mail and phone calls. mPulse is currently working with over 30 Managed Care Organizations across more than 20 states within different phases of their redetermination efforts to support engagement on all channels and channel combinations.
Personalization: After selecting your channels, be sure the messages you are sending are personalized and relevant to the member. Even if you are using pre-approved language for your redetermination outreach, make sure your salutation and any other merged fields are in the proper case and not all caps. Even an Excel novice can easily convert cells in all caps to proper case by applying a =PROPER formula to your selected cells. Proper case is easy, but what about language preferences? Reaching your Limited English Proficient (LEP) members can be difficult, especially when you don’t know who they are or what their preferred language is. For example, mPulse technology allows for you to go beyond typical language challenges or compliance required taglines by automatically transitioning between English and Spanish in our two-way SMS conversations.
Branding: Brand awareness and recognition leads to trust. You want your members to automatically know who all messages are coming from so they will not only trust it but also complete the desired request or action. Consider other communications that may be coming from your organization around the same time and coordinate your naming conventions to maximize brand awareness. Help get your brand on the right side of the inbox or in their known contacts by encouraging your members to store your phone number or SMS short code on their device or enhance those efforts by deploying mPulse Virtual Contact File (VCF) messages.
The New Normal for Medicaid
The return to normal, or rather the return to the new normal is here, and there is no slowing it down. This is still uncharted territory with a lot of work yet to be done, but if we have learned one thing here today, it is that working together, maximizing resources, and leveraging technology to provide a personalized member experience will be the key to successful redetermination efforts.
For more insights into how to deliver this experience to your medicaid population, view our on-demand webinar series for Redetermination.




