Automation and Consumer Expectations
Automation and digital technology have helped transform the way that we navigate healthcare as consumers, allowing for faster, higher-quality access to information and resources at scale.
Automation technology has also served to deliver significant operational efficiencies across the healthcare ecosystem, freeing up skilled human resources to focus on complex issues that require judgment and empathy for successful resolution.
As automation continues to shape member and patient engagement, consumers expect healthcare organizations to maintain a careful balance – provide them with easy, automated ways to access information when they need it while providing fast, direct access to people who can help them resolve difficult problems.
According to Gartner, when brands fail to create these rapid, seamless experiences, 96% of consumers will become less loyal1.
For businesses, using skilled staff for tasks that are better performed by automated tools increases costs, wastes patient time, and distracts staff from solving more complex and high-value issues. When automated tools are the only source of help for consumers, they are frustrated and disappointed when they reach the limits of the tool’s capabilities and are unable to receive quick, competent human assistance2.
Creating an optimal member experience as a health plan is a tremendous challenge. Modern consumers want personalized help, but only when they want it. Otherwise, they’d prefer to self-serve at the pace and intensity that they prefer through digital tools, or by googling their question3,4,5. For example, members expect that if they are going through a complicated referral, someone will be there to talk with them as soon as they need help.
However, for that same member, if they have to call and wait on hold to find out something as simple as the nearest pharmacy to them or the status of a refill, they can be frustrated by the length and difficulty of receiving human help.
Balancing Automated and Human Experiences
Truly effective and efficient healthcare consumer engagement requires utilizing both automation and human support to their full potential. The reality is that consumers expect to dictate which type of interaction they need and receive it quickly and affordably.
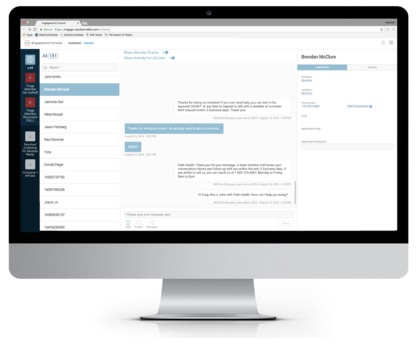
mPulse specializes in helping our partners create exceptional and delightful healthcare consumer experiences through the use of robust and effective automated tools in combination with The Engagement Console, our direct-to-consumer communication tool. The Engagement Console allows staff to have direct conversations with consumers via text message at scale by empowering them to manage multiple conversations at once.
What is The Engagement Console and how does it work?
 The Engagement Console is a secure, web-based application that enables staff to communicate directly with members via SMS. The Engagement Console allows staff to find specific individuals and either continue or initiate direct text message conversations with them.
The Engagement Console is a secure, web-based application that enables staff to communicate directly with members via SMS. The Engagement Console allows staff to find specific individuals and either continue or initiate direct text message conversations with them.
Staff can review individual member message histories for up to a year, providing essential context that saves time and frustration for both the member and the staff.
Common use cases for The Engagement Console include member support and services (essentially the same function as calling the member services phone number with a question, except The Engagement Console enables members to ask those questions via text message), pharmacy teams coordinating Comprehensive Medication Reviews, Care Managers tracking and support specific members, and routine administrative work such as appointment scheduling.
How does The Engagement Console enhance automated member journeys?
mPulse delivers automated Activator programs designed and delivered on behalf of clients to support members across their healthcare journeys. These automated digital programs handle 90-95% of incoming member messages without any need for intervention or review by a person.
For the other 5-10% of messages that need human support and problem solving, we have several different ways of making sure those messages get to member support staff for timely triage and resolution.
We’re able to do this by associating certain key phrases with alerts within The Engagement Console that tell staff that someone needs their time and attention.
 Common use cases are when members ask “Can someone call me?” – we would want to respond back to that message with a couple of options for the member: “You can reach us at 1-800-555-1234 from 8am to 8pm, 7 days a week. Or, if you’d like to talk with someone through text message, reply “AGENT” and a team member will follow up with you within 3 business days.”
Common use cases are when members ask “Can someone call me?” – we would want to respond back to that message with a couple of options for the member: “You can reach us at 1-800-555-1234 from 8am to 8pm, 7 days a week. Or, if you’d like to talk with someone through text message, reply “AGENT” and a team member will follow up with you within 3 business days.”
When a member then texts in the keyword “AGENT,” they receive a response setting expectations for follow up at the same time that a special triage alert is sent directly to The Engagement Console users informing them that a member needs their help.
We provide these instructions at key places throughout our automated journeys, particularly whenever we think there’s a high likelihood the member has a complex need. This lets members indicate that they want further follow up and then receive it in the same text message conversation as the automated program. This helps with brand recognition and trust while it trains members to use the channel as a direct access to member support services.

More Conversations in Less Time: Improving Member Experience with 1:1 Engagement
Leading healthcare organizations are redesigning their call centers to improve consumer experience and achieve operational efficiency. Learn to equip your support staff with 1:1 manual texting to harness SMS messaging for personalized service.
How does this support health plans?
The Engagement Console is a powerful efficiency tool, because it allows staff to manage multiple conversations simultaneously without requiring any members to wait on hold or requiring the member and the agent to be on the same phone call at the same time.

According to research conducted with our partners and clients, support staff can handle roughly 3x the volume of requests using The Engagement Console that they can use on the phone.
The reason why is simple: you’re working from a holistic text messaging history, you have digital tools to help you manage multiple conversations and keep track of them, and you do not have to wait (in real-time) for members to provide information while you, or they, sit on hold.
Why prioritize The Engagement Console as a product?
Our automatic replies are meant to handle as many different types of classifications of inbound messages as possible, and we have a robust library of different types of input and different suggested outputs to handle dozens of different types of questions, concerns, or barriers to action.
For 90-95% of member messages, our natural language processing will appropriately classify and respond to the message, addressing the need expressed by the member. However, the situations that require a human touch are often some of the most complex and important problems that members need help resolving.
Keeping in mind that these edge cases require extra attention and time, but create disproportionate value from a member experience perspective, shows a clear need to enable swift, intelligent identification of these conversations and offer tools that can help support the successful servicing of those member needs.
 In conclusion, the integration of automated tools with personalized, one-on-one digital outreach is essential for creating exceptional healthcare consumer experiences. At mPulse, we understand the importance of this balance, having dedicated over 12 years to developing advanced technology solutions that enhance member engagement while providing greater operational efficiency.
In conclusion, the integration of automated tools with personalized, one-on-one digital outreach is essential for creating exceptional healthcare consumer experiences. At mPulse, we understand the importance of this balance, having dedicated over 12 years to developing advanced technology solutions that enhance member engagement while providing greater operational efficiency.
By leveraging tools like The Engagement Console, our healthcare partners are better able to meet modern consumer expectations, resulting in improved health outcomes and increased member retention.
The effective combination of automation and direct member engagement tools not only reduces operational costs but also ensures that skilled staff are better able to focus on complex issues that require human judgment and empathy. This dual approach ultimately strengthens the relationship between health plans and their members, fostering trust and satisfaction in an increasingly digital world.





