Three years after the start of the COVID-19 pandemic and after over two years of continuous Medicaid enrollment, we finally saw the return to normal operations in April 2023 as the national public health emergency (PHE) was officially decoupled from Redetermination.
Now, almost 180 days out from the start of the unwinding process, it’s time to look back at how states have handled this massive undertaking, how Medicaid beneficiaries have fared, and the strategies of those plans who have been successful with the redetermination process these last six months.
The 2023 Medicaid Redetermination Process So Far
Having been in Phase 1 of the unwinding process (outreaching to members for updated contact information) for the majority of 2022 and into 2023, the market finally saw a shift into phase 2 in April 2023 when states officially began the process of redetermining eligibility for millions of members
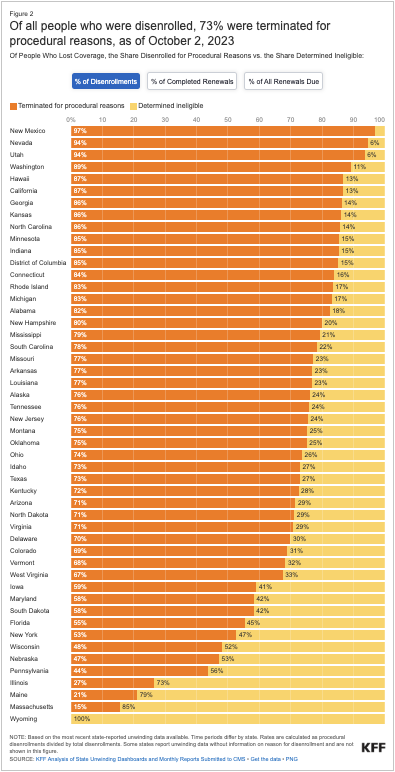
While it’s true that it was expected many people would lose their coverage, we are unfortunately seeing large numbers of people losing coverage for procedural reasons rather than due to a lack of eligibility. Recent data from the KFF Medicaid Enrollment and Unwinding Tracker shows that of the over 7 million people who have lost their Medicaid coverage since the start of the unwinding, 73% of those fall into this bucket of people losing coverage not as a result of merit or financial requirements but rather on a lack of replies, incomplete information, and the like.
In light of this, Congress has paused the redetermination efforts of 30 states due to their exceedingly high numbers of procedural disenrollments. Nearly half a million individuals will be reinstated after CMS found some states processing eligibility checks at the family level thus leaving out children who have lower or fewer requirements for coverage.
These 30 states have had to return to Phase 1 and 2 efforts to reach out to individuals to update their contact information and process their eligibility. Some are taking action to re-enroll everyone they presume might no longer be eligible, while others are asking their members to re-enroll based on their initial enrollment month.
An All Hands On Deck Approach
There’s been no shortage of assistance from state and federal organizations providing guidance and resources on approaches to drive the redetermination process and encourage people to re-enroll and maintain as much coverage as possible.
Furthermore, to reduce some of those procedural issues, health plans are now also allowed to help individuals fill out enrollment forms, which we hope will drastically reduce the amount of procedural disenrollments.
Another game-changing move was a declaratory ruling by the FCC earlier this year that health plans can now leverage SMS texting and IVR calls to conduct outreach and support continuation of coverage efforts.
This brings us to a discussion around digital strategies and asking the question, will doing the same thing deliver different results? If states are encountering issues around procedural disenrollment, what other approaches can they adopt?
Digital Strategies to Tackle Medicaid Redetermination
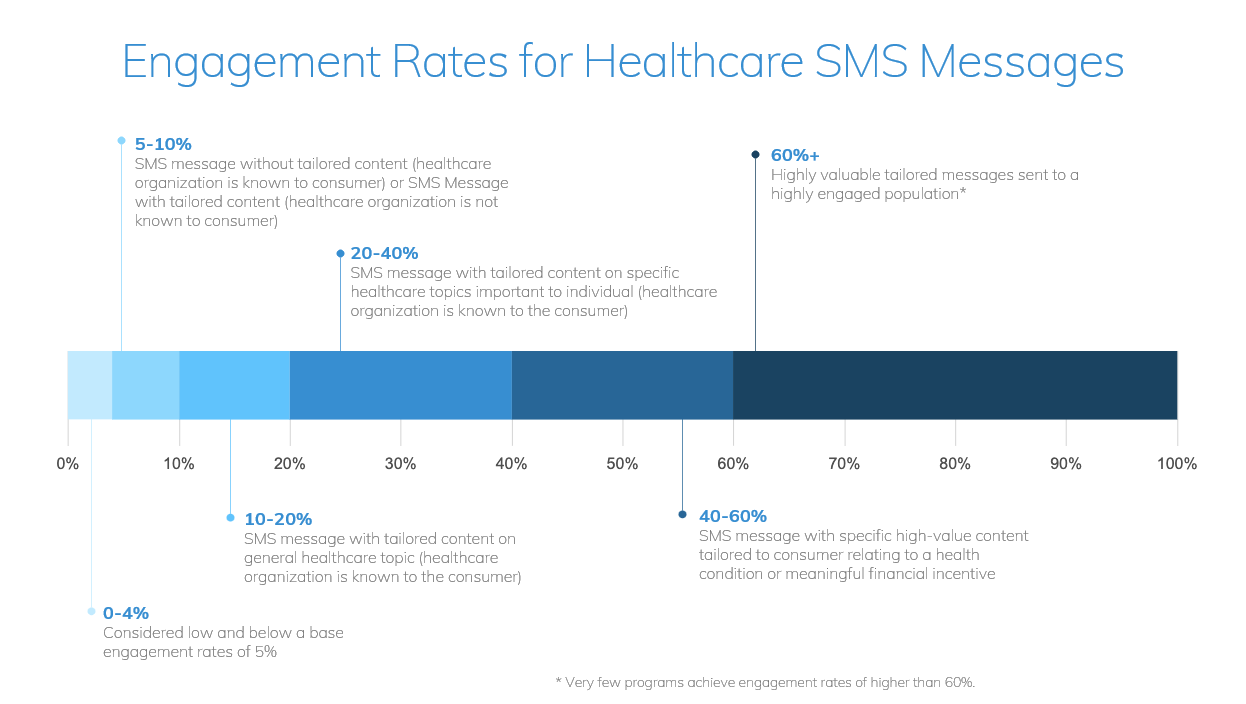
If traditional outreach methods haven’t been as effective as we hope in some states, it only makes sense to consider alternate strategies when it comes to member outreach. One channel we have seen work very successfully in redetermination efforts is SMS texting. A widely adopted channel, it can produce engagement rates of up to 60% for the most valuable and tailored programs sent to engaged populations.
To employ the SMS channel in your redetermination efforts, there are four best practices to consider.
Deliver Outreach Aligned to Language Preferences
Be sure the messages you are sending are personalized and relevant to the member. Reaching your Limited English Proficient (LEP) members can be difficult, especially when you don’t know who they are or what their preferred language is. Even if you are using pre-approved language for your redetermination outreach, an easy action to implement when leveraging a text channel is to ensure you align your messaging to the language preferences of your members. For example, mPulse technology allows for you to go beyond typical language challenges or compliance required taglines by automatically transitioning between English and Spanish in our two-way SMS conversations.
Include Educational Content to Address Health Literacy Gaps

Use captivating and engaging content in these outreach programs that educate individuals on why they should reapply. While creating awareness is the first step, educating members on why it’s important to reapply in an effort to maintain their coverage is vital. Think about it: if you don’t understand the benefits of Medicaid and how it contributes to your long-term health, why would you spend the time and energy filling in forms to prove your eligibility? Providing members with educational tools designed to build knowledge and confidence will increase the likelihood that they’ll take action.
Incorporate Behavioral Science Strategies into Messaging
Behavioral science has become a crucial component of health engagement programs and has been proven to directly impact health outcomes. Loss aversion, a cognitive bias that describes why the pain of losing is psychologically twice as powerful as the pleasure of gaining, or social proof, the phenomenon where we look around us for clues on how to behave, are examples of behavioral science strategies you can incorporate into messaging to foster greater trust, dispel concerns and increase the likelihood that your hard-to-reach members will engage and respond to outreach materials. This will help create a need for members to act.
Use Conversation AI Outreach to Identify Barriers
Leverage conversational AI and two-way texting to uncover barriers and encourage action. These AI powered, bidirectional texts allow automated, tailored responses to address individual barriers. If members reply to the texts, conversational AI uses natural language understanding (NLU) to “listen” for known barriers and other expected replies and provide relevant, automated responses to create logical conversation flows to address these barriers. This is also an opportunity to build health literacy and raise awareness about the need to maintain coverage. You can imagine how helpful these kind of capabilitiies are when trying to determine barriers to reapplying for coverage and encouraging action among your members.
An Activation Solution
While organizations may feel hampered by the requirement to use pre-approved state language, there’s no reason you can’t use it as an interim solution or in tandem with additional, tailored outreach.
This is exactly the approach that one health plan adopted in preparation for the unwinding. Their goal was to activate Medicaid members with high-impact messaging and content to educate, set intent, and reduce the perceived effort of completing the redetermination process.
They achieved this by utilizing automated two-way programming to uncover and address member barriers, integrating fotonovelas, in multiple languages, into the outreach messaging. They delivered relatable stories to members that leveraged the endowment effect and loss aversion to build intent to keep coverage, and they used natural language understanding (NLU) to uncover and address common barriers and address members’ issues at scale.
As a result, 33% of targeted members engaged with the program and by leveraging NLU, 18% of targeted members responded to the program which uncovered and addressed common barriers.
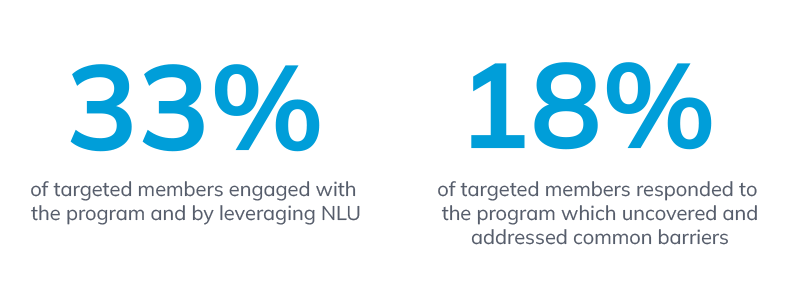
So, what does this prove? SMS is an effective channel for member outreach. It allows for delivering messages via a high-reach, high-touch channel and gives people something they can either act on in the moment or return to after the fact.
In the example above, the outreach was delivered in both English and Spanish, and made all the difference in overcoming barriers to action. Considering the best practices for member outreach that we mentioned earlier, it’s clear that addressing people in their own language, at the right time, on the right channel is key.
Looking Ahead to Better Health Coverage
While procedural disenrollment is a concern, several systemic issues have been identified, and the administration is taking steps to address them to keep people connected to care. Better processes and partnerships are expected to come into play, enabling easier approvals and ways to share data between states and health plans.
This includes partnering with managed care organizations, community health workers, walk-in centers, and more to raise awareness and assist enrollees in completing and submitting their renewal forms, even over the phone.
And while state-based content and language is a great starting point for communication, if you’re looking for ways to enhance your outreach efforts, start by considering what’s worked, what hasn’t worked, and where you can integrate these best practices to produce better outcomes.
How can you improve the content, add more languages, or add additional outreach modalities such as phone, email or SMS? Most importantly, how can you include streaming content and facilitate two-way conversations to overcome barriers and inspire your member populations to take action?
Not sure where to start? Reach out to learn more about the power of SMS and how you can establish a robust redetermination solution to reduce coverage loss and create high-value member touchpoints.






