Health plans are embracing digital strategies to deliver personalized interventions at touchpoints along consumer health journeys. Digital technology has the potential to bring together automated outreach and drive awareness of self-service capabilities to support a variety of healthcare consumer needs. When executed well, it enables organizations to rapidly respond to consumer actions and inflection points, which is a critical element of delivering an impactful consumer experience and improving business outcomes.
Health plans’ ability to innovate the digital consumer experience is driven by:
- Their organizational agility.
- Their technology stack.
- The quality of their consumer data.
The more capable the technology and the better aligned their core consumer databases are to their consumer experience strategy the more successful they will be.
Personalization requires actionable insights about the consumer and connected digital capabilities to deploy touchpoints that both align with the insights and are delivered to the consumer within a timeframe that ensures the experience is relevant.
Achieving this is a broad goal for most health plan’s digital strategy- insights powered orchestration of personalized digital touchpoints powered by a centralized consumer dataset.
The health consumer journey consists of a series of touchpoints that span clinical, health engagement, marketing, customer service and administrative areas.
Non-healthcare specific technologies- such as customer relationship management systems (CRMs), marketing automation, contact center tools and digital experience platforms (DXPs)- are deployed at the departmental level and coordinate some of these touchpoints, but have limitations for managing the complexity of clinical and healthcare-specific experiences.
The challenge for health plans is that many of the most important consumer touchpoints are clinical and administrative related and are powered by legacy systems that were designed to capture transactional records and not to build rich consumer insights – or relationships.
Technology vendors can often solve for specific needs or offer point-solutions within the consumer health journey, but when these vendors are combined it creates a fragmented technology system, one that is almost impossible to innovate around at a macro level and does not enable the development of a centralized consumer dataset to power more advanced enterprise engagement strategies.
Health Experience Innovation
Collaborating with leading health plans and industry experts mPulse has launched Health Experience and Insights (HXI).
Through strategic acquisitions and technology innovation, mPulse has connected foundational digital engagement technologies with AI-powered predictive analytics to power the advanced personalization needed to optimize the healthcare specific experiences throughout the consumer health journey.
HXI is designed to deliver a more personalized consumer experience that delivers better health outcomes and creates improved operational efficiency.
Using predictive analytics and connected digital experiences health plans can anticipate the needs of individuals throughout the consumer journey and launch optimal personalized digital experiences quickly and efficiently. It ensures the consumer receives the personalized digital experience that supports and empowers them along their health journey.
It also enables health plans to optimize consumer touchpoints with high priority departmental goals- such as member onboarding and retention, HEDIS and CAHPS performance, care management touchpoints, and driving adoption of strategic technology investments such as health portals.
Health Engagement Innovation
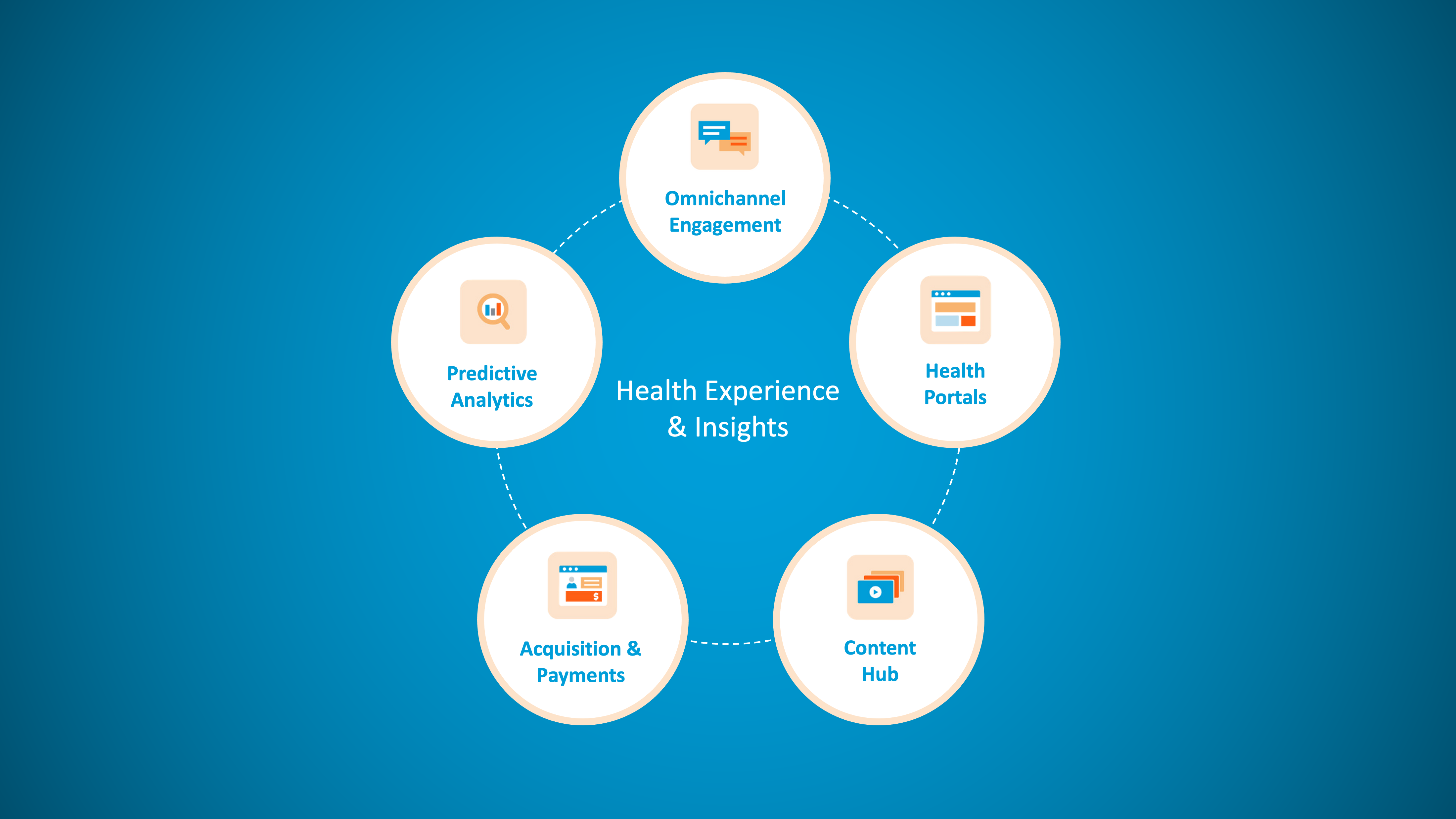
There are four capability drivers for HXI:
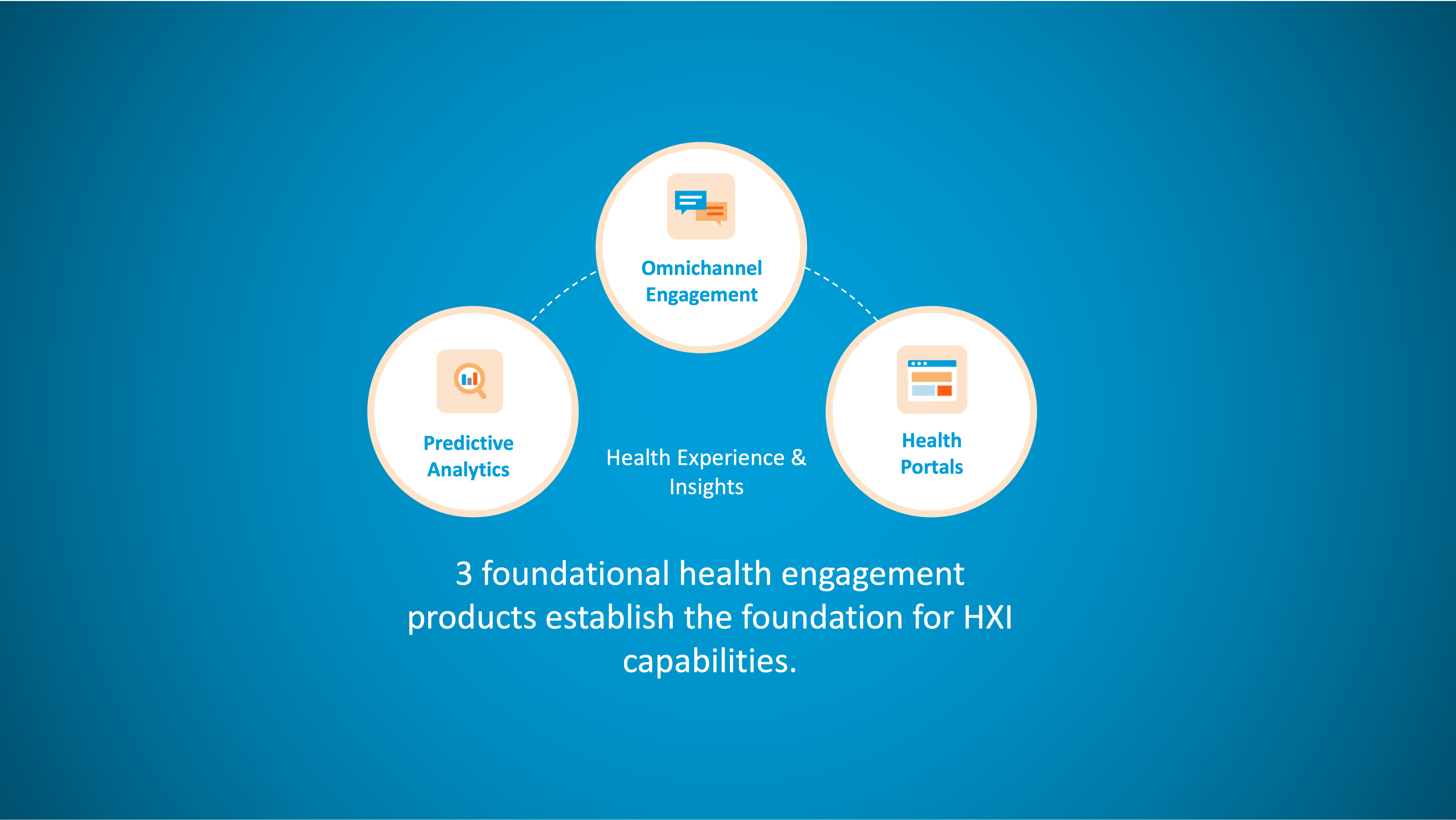
1. Three Foundational Products
HXI connects three core health plan technologies into a single ecosystem- Health Portals, Predictive Analytics and Omnichannel Engagement. Each area is a foundational capability for health plans, and when connected they have transformational potential. Which is why mPulse has brought them together as an industry first. A key feature of HXI products is composable deployment, so health plans can select the capabilities they need to deliver an HXI vision aligned to their existing technology investments.
2. Consolidation of Vendors
A range of technology vendors supporting different touchpoints along the consumer health journey creates multiple risk profiles for the health plan and creates organizational complexity. Deploying a single vendor for HXI products creates a single risk profile, reduces complexity and immediately establishes connected capabilities throughout the whole consumer journey.
3. Connected Data Layer
Arguably the most powerful element of HXI is the connected data. It centralizes, connects and standardizes preferences, experiential, demographic, health status, and predictive risk data ingested and captured across our product sets. It is built of dynamic, member profiles shared across products that capture insights at each digital touchpoint including clinical and health engagement areas.
The member profiles feed into predictive analytical models to create a single data environment that enables advanced closed loop analytics. Consumer experience (CX) technology systems across any industry require centralized, structured and actionable consumer data. It is the same for health plan CX use cases. HXI promises the opportunity to achieve this for high value clinical and engagement use cases.
4. Powering Advanced Digital Engagement Capabilities
The connected HXI products and digital experience data layer create a platform to realize value from advanced engagement capabilities. Next best action analytics, orchestration and AI-powered real time engagement strategies all become attainable with a centralized consumer data set and connected digital tools for rapid deployment of personalized experiences.
Foundational Health Engagement Capabilities
Health Portals
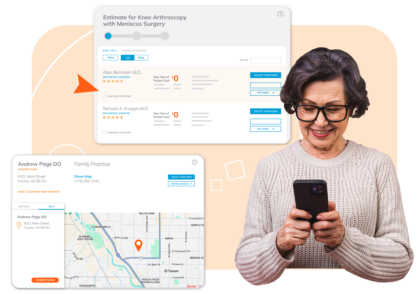
mPulse’s H30 Connect portal products have been in-market and used by leading health plans for over 20 years. H30 Connect products include member, provider, employer and broker portals.
The portals include a range of consumer-focused self-service capabilities across 50 modules, including- price transparency, prior authorization, provider search, billing, member statements, care team and engagement.
The H30 Connect portals Tap into over 100 different connectors to various industry organizations and systems using industry data standards.
Predictive Analytics

mPulse’s Decision Point Predict Analytics combines data transformation capabilities, AI-powered predictive models and data visualization tools to unlock actionable consumer insights. Launched in 2017 Decision Point Predictive Analytics is leveraged across a range of health engagement challenges across HEDIS, CAHPS and member retention.
By restructuring fragment data and enriching it with consumer data and social needs data, which are necessary when looking at the individual level, Decision Point models predict member behaviors and make recommendations on how they need to be engaged.
Omnichannel Engagement
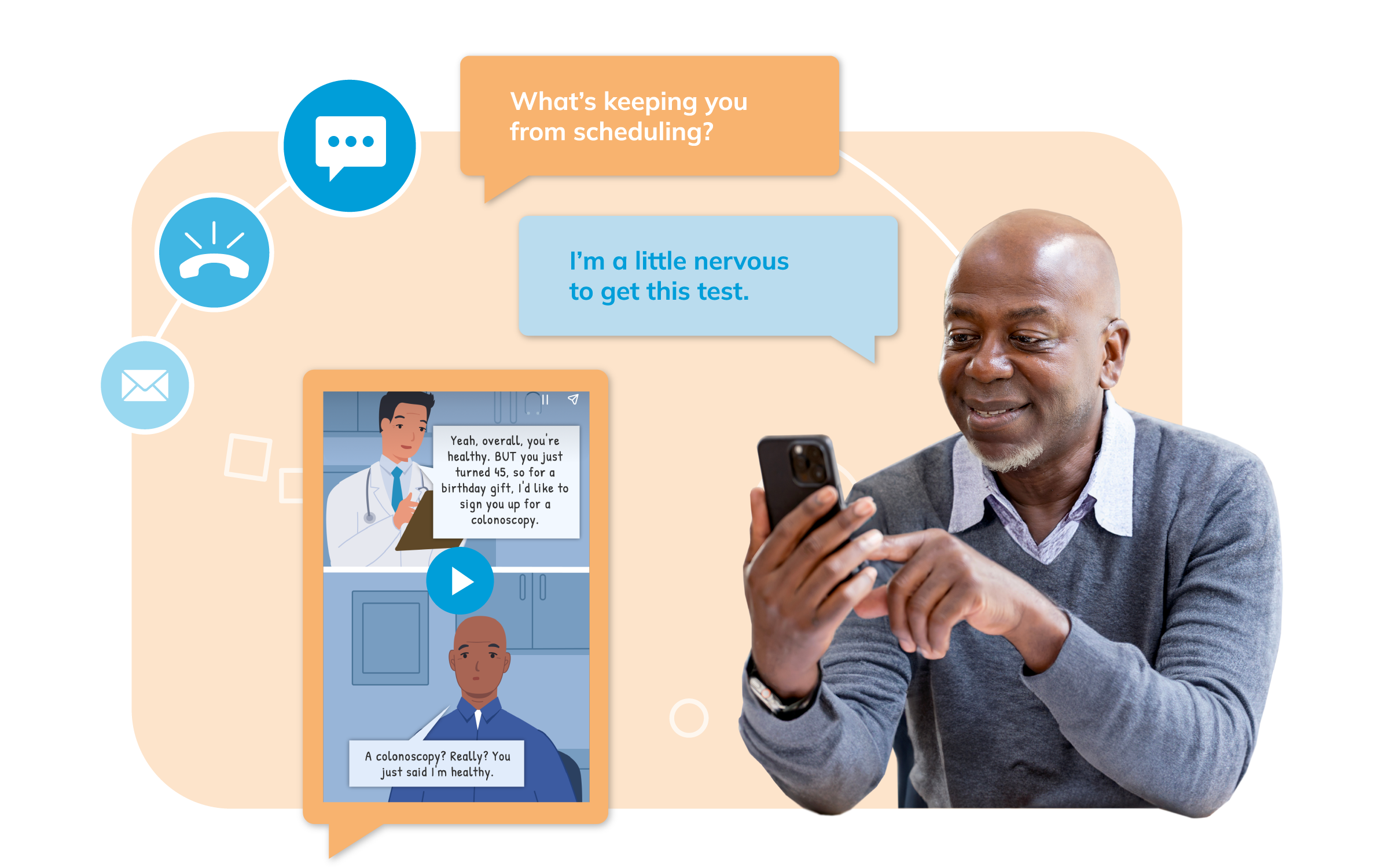 mPulse omnichannel engagement products enable efficient deploy of proven outreach and engagement programs that connect consumers to key resources and keep them on top of their health goals.
mPulse omnichannel engagement products enable efficient deploy of proven outreach and engagement programs that connect consumers to key resources and keep them on top of their health goals.
These programs use conversational AI to uncover barriers consumers may have and navigate them to resources and content to drive the completion of key health goals, and where appropriate leverage streaming content to address health literacy and challenges in self-efficacy. Versions of the programs are available that address the needs of hard-to-reach populations and individuals who face SDoH challenges.
Connected Products
The HXI ecosystem allows other products and capabilities that support the consumer health journey to be connected. These products benefit from insights about consumers that predictive analytics provides and HXI data more broadly so that consumer experiences can be personalized, and insights from consumer touchpoints in these areas can be captured.
mPulse has connected Acquisition & Payments and Content products into HXI developing other product areas that impact the consumer journey. Acquisition & Payments products provide early insights about members that can enable personalization of new member navigation experiences.
Content products are leveraged to deliver culturally sensitive and personalized content experiences to address key barriers and challenges people need to overcome at health journey inflection points.
Enterprise Efficiency
HXI capabilities are designed to align and integrate with existing health plan processes and systems. Structured consumer data can feed into other plan technologies to supplement marketing databases and provide consumer insights to contact center teams.
This provides important insights across a range of consumer attributes from preferences to which engagement programs they have received and whether or not they engaged. It is beneficial to marketing to know that a health plan consumer frequently engages with text outreach and opted out of IVR outreach.
Similarly, contact center staff benefit from insights about risk profiles of consumers and insights about challenges they experienced along recent touchpoints on their consumer health journey. Leveraged this way HXI data feeds can contribute to broader CX enhancements across other consumer touchpoints.
HXI generates a wealth of insights about who needs to be engaged, on what topic, when and what the best way is to engage them. When these insights are modeled alongside enterprise goal prioritization and budget targets, it enables robust orchestration of digital outreach and engagement to optimize overall organizational performance while creating significant operational efficiencies.
mPulse is sharing its HXI products and capabilities at its Activate 2024 conference in Dallas, TX September 24-26. The conference theme is From Insights to Intervention: Creating Consumer Centric Digital Experiences and includes a Keynote session by Dr Sachin Jain President and CEO of Scan Health Plan.

Health Experience & Insights Exploration Hub
Predict member risk. Engage intelligently. Streamline health navigation. Health Experience & Insights (HXI), our unified yet configurable product suite, connects predictive analytics, digital engagement, and health portals to redefine the healthcare experience.





