Medication adherence, while critical for managing chronic conditions like diabetes, high cholesterol, and cardiovascular disease, has still proven to be a struggle for many Americans. Studies show that adherence rates are declining, posing a significant challenge for healthcare providers and plans managing Medicare and Medicaid populations.
The Medicare Part D prescription drug program is also undergoing significant changes, presenting health plans with a number of new challenges and opportunities. With increasing Star rating cutpoints, new measures being introduced, and a focus on health equity, plans must adapt their strategies to drive better medication adherence and overall member outcomes.
The Part D Landscape
The Medicare Prescription Drug, Improvement, and Modernization Act (MMA) of 2003 established Part D, providing subsidized prescription drug coverage for seniors and people with disabilities. Since its inception, Part D has undergone significant changes, driven by a continuous effort to improve affordability and access to medications.
There are a number of key trends shaping the Part D market. Plans are increasingly focused on value-based care, aiming to deliver better health outcomes at lower costs. Medication adherence is a key metric in this equation, as it directly impacts patient health and reduces hospital admissions.
By carefully managing their formularies, Part D plans can also negotiate lower drug prices and offer cost-effective alternatives to beneficiaries. Many Part D plans have tiered structures, with lower copays for generic medications and higher costs for brand-name drugs as well as preferred value networks offering lower cost sharing to members. These designs encourage patients to choose more affordable options whenever possible.
The Adherence Challenge: Beyond Cost
While cost can be a barrier to adherence, it’s not the only one. Studies reveal a complex interplay of factors that contribute to non-adherence, including:
- Complexity of regimens: Managing multiple medications with different dosing schedules can overwhelm patients.
- Side effects: Concerns about medication side effects can lead patients to skip or stop taking their medication altogether.
- Health literacy: Limited understanding of medications and their benefits can hinder adherence.
- Lack of communication: Poor communication between healthcare providers and patients can create confusion and lead to non-adherence.
With that in mind, the Centers for Medicare & Medicaid Services (CMS) has implemented several key updates to the Part D Star Ratings program that plans need to be aware of.
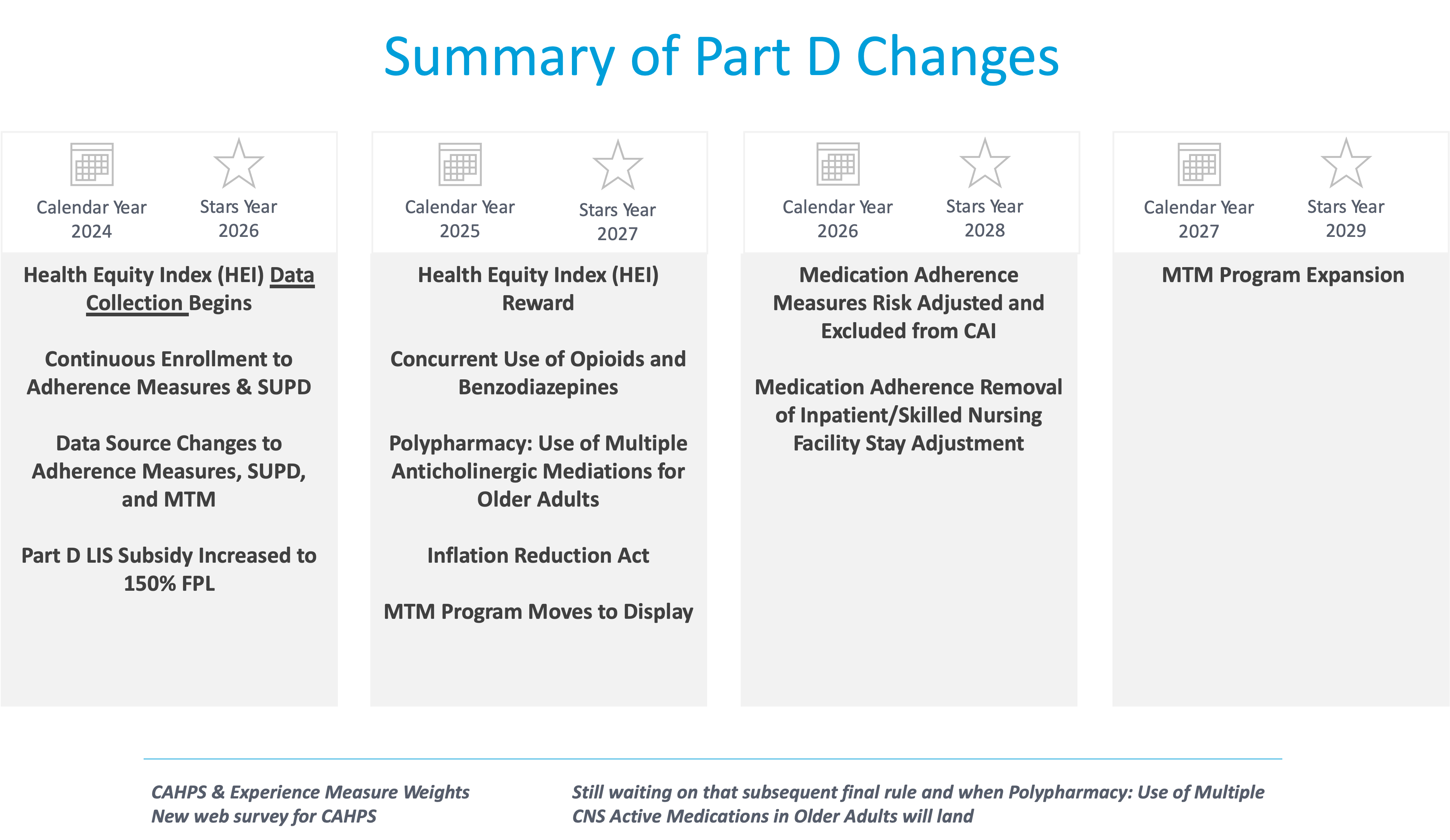
Year over year, the cut points to achieve 4 or 5 stars for measures like diabetes, cholesterol, and hypertension medication adherence have steadily risen. Plans that were previously assured of achieving their stars are now struggling to maintain or improve their star performance.
This year we’ve seen an increase in subsidy for the Federal Poverty Level (FPL). So some people who didn’t qualify for a low income subsidy last year may now qualify this year.
Two new patient safety measures have also been added for 2024 – concurrent opioid and benzodiazepine use, as well as polypharmacy utilizers. These bring new challenges in member engagement and education as we try to educate members on safety concerns or adverse reactions.
We’ll also see some significant changes in cost sharing for members with the Inflation Reduction Act, which will reduce out-of-pocket costs for many members, impacting medication adherence dynamics for plans, while the introduction of the Health Equity Index (HEI) and Reward factor for 2027 aims to close healthcare disparities by incentivizing improved outcomes for low-income, disabled, and dual eligible populations.
Perhaps the biggest challenge is the focus on adherence measures with a goal of 80% PDC. This is the gold standard when it comes to measuring adherence for diabetes, hypertension, and cholesterol drugs. For medication to be clinically effective, members must take it a minimum of 80% of the time it’s prescribed. Critically, adherence can impact other measures and performances too.
With these updates, plans must proactively identify barriers and tailor engagement approaches for specific populations and individual member needs.
Case Study: Improving Diabetes Adherence with Multichannel Outreach
To illustrate effective strategies for driving adherence, consider this case study from a Medicare plan that partnered with adherence program experts:
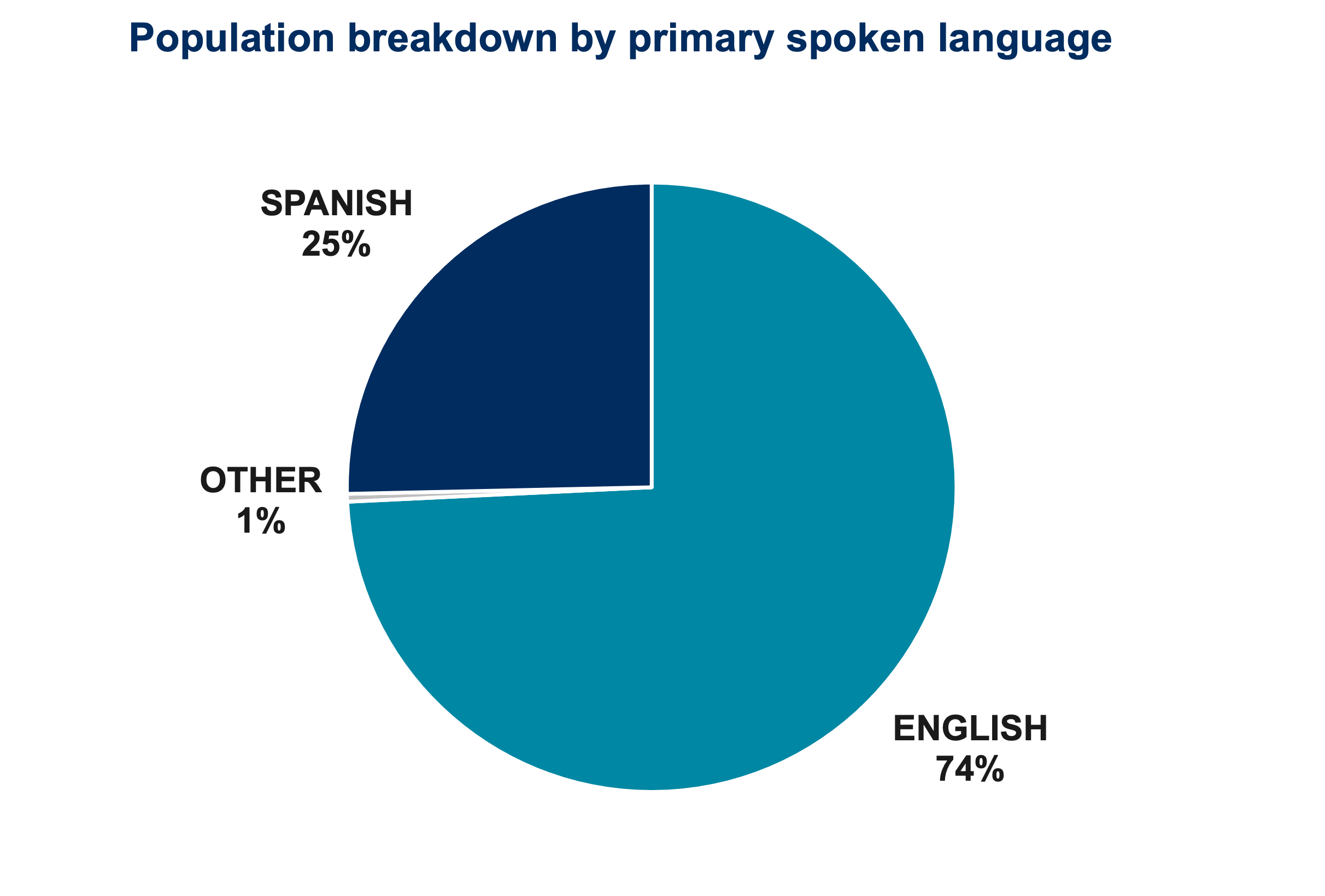 The Challenge: An mPulse partner with 14,000 members noticed that 25% of the adherence population had Spanish listed as their primary language. However, engagement rates with this Hispanic population were lagging for key adherence measures like diabetes, cholesterol, and hypertension medications.
The Challenge: An mPulse partner with 14,000 members noticed that 25% of the adherence population had Spanish listed as their primary language. However, engagement rates with this Hispanic population were lagging for key adherence measures like diabetes, cholesterol, and hypertension medications.
The Approach: The plan translated its English language text messaging adherence campaigns into Spanish to improve relevance and language preferences. This was combined with mailings, calls with interpreter services, and other multichannel outreach tailored for this population.
The Results:
- Participation rates among Spanish speakers increased by 9%
- Spanish members who texted were 10% more likely to engage over the phone
- 90-day prescription conversion increased by up to 40%
- Treatment rates rose 1-4% across the three adherence measures for the overall population
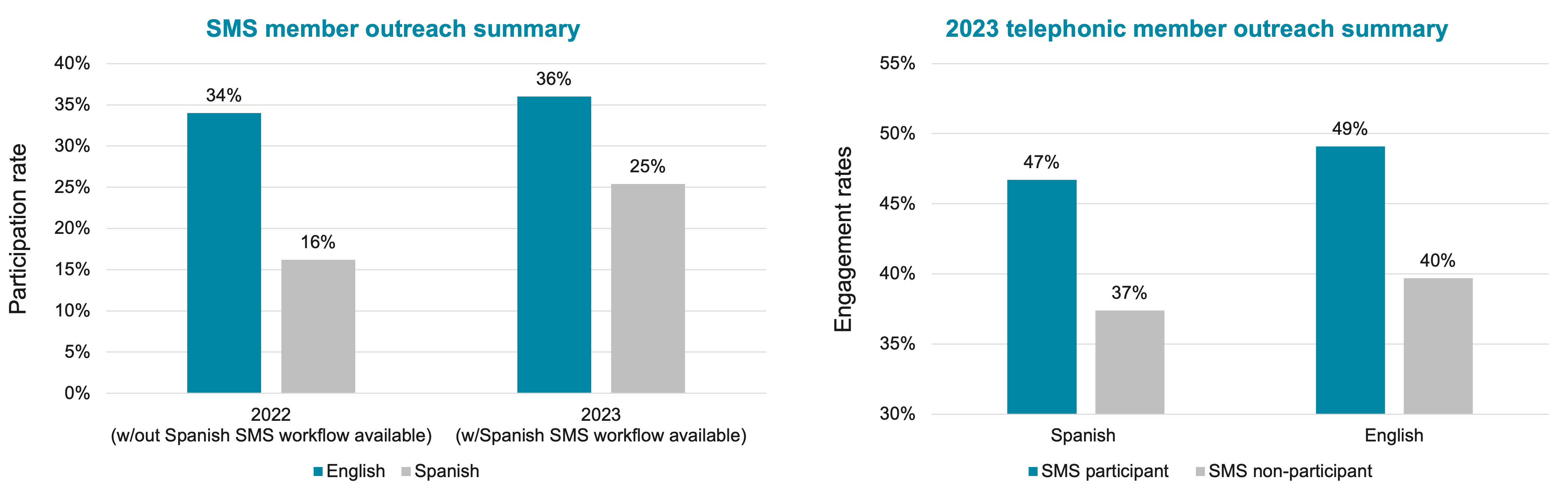
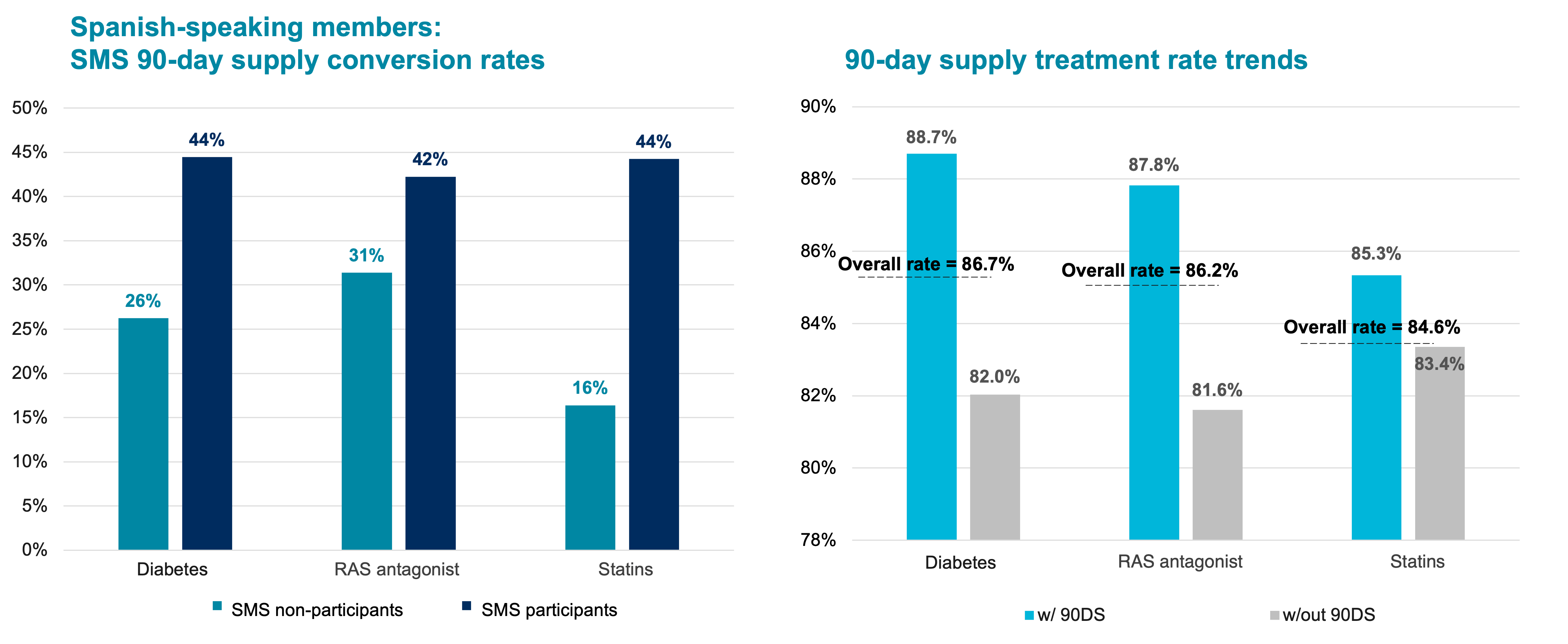
By recognizing linguistic needs and innovating with multichannel digital outreach, this plan boosted engagement and adherence for an important subpopulation and positively impacted compliance rates across the entire population. Texting capabilities provided an efficient way to expand their outreach scope without heavily increasing resources.
Weaving Clinical Insights into Member Engagement
While the tactics and channels were impactful, this program’s success hinged on marrying smart engagement with clinical insights. The team identified and resolved common barriers like:
- Access issues in getting medications or seeing providers
- Low health literacy on why adherence matters
- Financial concerns around medication costs
By adopting a targeted, multi-channel approach that addresses the specific needs of each patient, they were able to ensure the right message was delivered through the right channel (phone, text, email) at the right time.
Helping patients overcome barriers like transportation or lack of a primary care physician can be crucial for long-term adherence and can significantly improve engagement and experience. Rich, streaming content provided immersive, educational content that was helpful in resolving some of those barriers and providing a quick and easy way to “click to care” via a mobile web experience.
Leveraging technology also meant that automated systems could handle routine tasks, freeing up healthcare professionals to provide more personalized support to high-risk patients.
Addressing Risk through Advanced Analytics
One area of significant opportunity for plans is leveraging advanced analytics and machine learning to better identify and engage high-risk members before they become non-adherent. Key factors like socioeconomic indicators, health risks, prior-year adherence patterns, and claims data can be used to precisely predict each member’s likelihood of achieving adherence goals for the coming year.
With this predictive risk scoring, plans can tailor the intensity and channel mix for outreach programs. For example:
High-Risk: Direct phone outreach plus automated reminders and messaging via text/email
Lower-Risk: Light-touch text/email reminders and engagement prompts
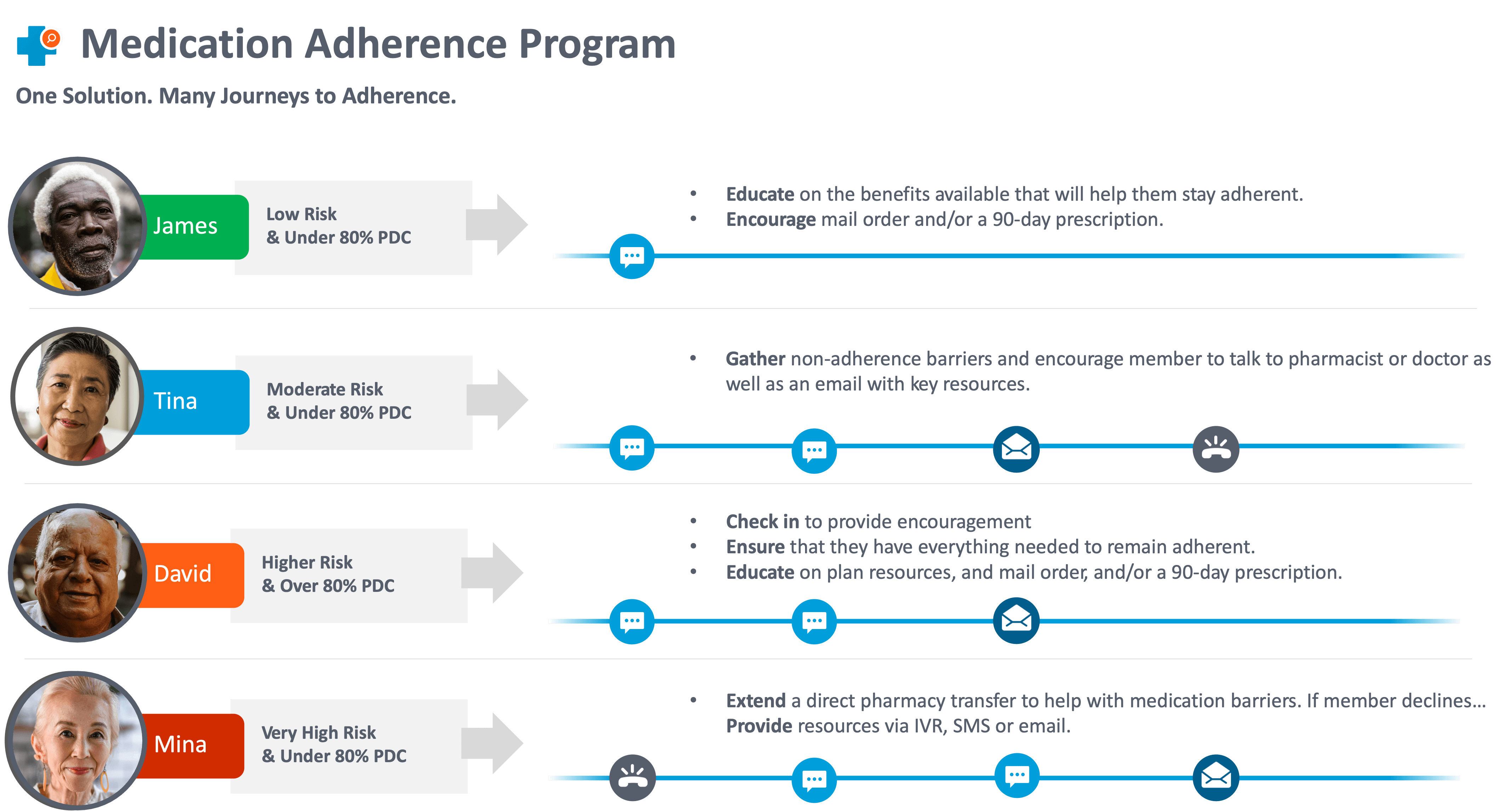
By frontloading resources on those most likely to miss adherence targets, plans can optimize resources while nudging all members toward adherence. Continuous monitoring allows risk scoring to be adjusted throughout the year based on response patterns.
This type of advanced targeting is a powerful new capability that helps plans cost-effectively keep members adherent and improve outcomes.
As Medicare plans navigate rising performance bars and new incentives around health equity, medication adherence will remain a crucial priority. By adopting a targeted, multi-channel approach that addresses the specific needs of each patient, healthcare providers and plans can clear these hurdles and drive better health outcomes across all populations.