On August 25, the Centers for Medicare and Medicaid Services (CMS) announced that it is discontinuing Direct Enrollment for performance year (PY) 2026.
Here’s an overview of what carriers should know:
When does this update take effect?
CMS’ SDE service will be disabled on October 31, 2025.
What should carriers do to prepare?
Carriers who relied on Standard Direct Enrollment (SDE) must transition to EDE to avoid disruption. A carrier that fails to implement an EDE pathway will not be able to assist consumers with enrollment via its website. This would likely result in the loss of new enrollments and the inability to service existing Marketplace plan members directly through a digital channel. Consumers would need to be directed to HealthCare.gov or an approved EDE entity to complete their applications.
 According to CMS, carriers must complete the following steps:
According to CMS, carriers must complete the following steps:
- Transition to EDE: All enrollment activities must be conducted using the Enhanced Direct Enrollment (EDE) functionality after October 31, 2025.
- Modify processes: If a carrier uses a Classic Direct Enrollment pathway on an EDE website, its processes must be updated to exclusively use the EDE features.
- Integrate with CMS APIs: Carriers participating in EDE must build a platform that integrates with a suite of more than 20 APIs from CMS to manage eligibility, enrollment, and post-enrollment activities.
- Undergo third-party audit: Primary EDE entities must pass an extensive third-party audit of their application and privacy/security structure.
- Seek CMS approval: The EDE application and platform require approval from CMS. Carriers must also comply with ongoing monitoring.
- Refer consumers to EDE: If a carrier has an approved EDE platform, it must refer consumers to that platform or other approved EDE partners. There is no longer the option to redirect consumers to the classic pathway.
- Partner with existing EDE entities: Carriers that do not want to build their own EDE platform can become an “upstream EDE entity” and leverage a platform built by a primary EDE entity.
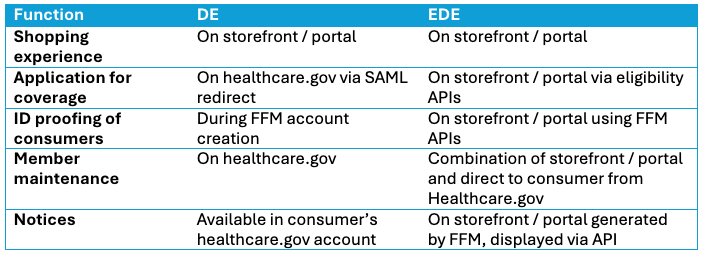
What is Standard Direct Enrollment (SDE) vs Enhanced Direct Enrollment (EDE)?
In short, EDE removes the need for health consumers to navigate between healthcare.gov and the health insurer’s website when enrolling in a health plan. EDE is a program in which CMS provides direct enrollment (DE) organizations, such as carriers, a set of Application Program Interfaces (APIs) that allows organizations to communicate information about a consumer to the Marketplace and allows CMS to communicate information about a consumer back to the partner.
Why EDE?
EDE offers health plans several advantages, including:
- Subscriber acquisition & retention: EDE is like having your own brick-and-mortar retail store dedicated to your products and only your products, rather than being one shop out of hundreds at the mall. EDE encourages your prospective subscribers, enrollees, and potential members to shop for only your health plans.
- Consumer experience improvements: For health consumers, shopping, applying, and enrolling in health insurance can be a confusing experience wrought with friction. Creating a one-stop-shop for consumers to take all the steps of shopping and enrolling in a health plan creates a simpler, more consumer-friendly experience.
- Consumer insights: EDE allows health plans to capture consumer analytics along their shopping, applying, and enrollment journey. This data can be used by plans to optimize their UI, consumer acquisition, and enrollment strategy.
- Broker relationships: EDE enables brokers to do their jobs more efficiently and better serve their clients through a simpler, more user-friendly online enrollment process.
- Operational efficiency gains: EDE reduces the administrative burden on health plans to operate the on-exchange enrollment process.
How does mPulse’s EDE solution work?
mPulse is a CMS-approved partner for EDE. Our EDE solution works like this:
For Carriers
- mPulse sets up an online shopping and enrollment portal on behalf of the carrier to be used by its health consumers and brokers when they enroll in on-exchange and off-exchange plans
- Carriers can encourage their members, brokers, and health consumers to shop and enroll in a health plan, renew an existing plan, and update their enrollment
Individual subscribers
- Can renew their plan
- Can update their enrollment
- Can reverify their eligibility
Brokers
- Can shop for and enroll in plans on behalf of their clients
- Can actively renew their clients
- Can update enrollment on behalf of their clients
What are the takeaways I should know about EDE?
EDE is an impactful way to set your organization up for success today and beyond. It gives health plans your own storefront and allows you to improve relationships with consumers and brokers while boosting subscriber enrollment and retention.
Connect with one of our mPulse EDE experts to learn more.

What is HXI?
Discover how Health Experience Insights (HXI) transform engagement strategies—this strategic resource breaks down the core pillars of HXI and how it drives better health outcomes.





