
CMS Interoperability Rules: Why Health Plans Shouldn’t Wait to Prepare
The Centers for Medicare & Medicaid Services’ CMS-0057F interoperability and prior authorization rule marks a major shift in how health plans manage compliance and member care. While the most complex requirements don’t take effect until January 1, 2027, the reality is that preparation needs to start now.
Why? Because this rule isn’t just another compliance exercise. Done right, it’s an opportunity to streamline operations, improve member and provider experiences, and strengthen competitive positioning.
In this guide, we’ll break down the key CMS-0057F requirements, outline the steps you can take now, and show why forward-thinking plans will come out ahead.
Key Requirements & Deadlines
The CMS-0057F rule applies to state Medicaid and CHIP agencies, Medicaid and CHIP managed care plans, Medicare Advantage organizations, and Qualified Health Plan insurers on federally facilitated exchanges. Even if you’re not directly impacted today, commercial payers should take notice — these standards could expand to other lines of business.
Here are the core changes and when they take effect:
Prior Authorization Decision Timelines (2025)
- Standard requests: response required within 7 calendar days.
- Expedited requests: response required within 72 hours — and in some urgent cases, within 24 hours.
Denial Reason Transparency (2025)
- Plans must provide clear, specific denial reasons to help providers understand next steps.
Reporting Requirements (2026)
- Public-facing prior authorization metrics (approval rates, turnaround times, volumes).
- CMS-facing reports on Patient Access API usage.
Implementation of Five New FHIR APIs (2027)
- Provider Access API – Enables providers to access member health data directly from their EHR.
- Payer-to-Payer API – Facilitates data sharing when members switch plans or have dual coverage.
- Coverage Requirements Discovery API – Helps providers determine if prior auth is needed before submitting.
- Documentation Templates & Rules API – Guides providers through required documentation directly in their EHR.
- Prior Authorization Support API – Submits requests electronically with all required information.
Breaking Down the Five New APIs
While these APIs are technical in nature, their intent is straightforward: make it easier and faster for providers and payers to share accurate information and reduce delays in care.
One of the most striking early findings from organizations piloting the Coverage Requirements Discovery API is a 60% reduction in unnecessary prior authorization submissions. That’s time, cost, and frustration saved — before the care journey even starts.
Together, these APIs are designed to:
- Shorten decision-making timelines.
- Reduce redundant or unnecessary requests.
- Improve the accuracy of submissions.
- Strengthen care coordination between providers and payers.
Five Steps to Implementation Success
The rule is complex — but with a clear plan, it’s manageable. Here’s where to start.
1. Assess Your Current State
Don’t just glance at existing workflows — audit them.
- Map end-to-end prior authorization processes: From request intake through decision and communication back to the provider.
- Measure actual turnaround times: Compare them to the new CMS requirements.
- Analyze denial reason documentation: Is it specific and actionable? Can providers clearly understand next steps?
- Review interoperability maturity: Which APIs are already in place from CMS-9115F, and how well are they performing?
Pitfall to avoid: Assuming your current process meets the new timelines without hard data.
mPulse POV: Use this stage to establish a performance baseline — it will be critical for both compliance reporting and proving ROI later.
2. Assemble a Cross-Functional Task Force
CMS-0057F implementation will touch every corner of your organization.
- Core members: IT, operations/utilization management, compliance/legal, provider relations, product, engineering, and vendor management.
- Why this matters: API deployment affects workflows in utilization management, the provider experience, and even communications.
- Add provider voices early: Whether through advisory councils or key partners, get feedback before you build to avoid low adoption rates.
Pitfall to avoid: Treating this as a purely IT-led project — operational buy-in is critical to ensure process alignment and provider adoption.
mPulse POV: We’ve seen implementation move faster when provider-facing teams and IT work in lockstep from the beginning.
3. Prioritize Your Roadmap
Not all five APIs will require the same level of effort or integration complexity.
- Identify dependencies: Some APIs, like Coverage Requirements Discovery, depend heavily on accurate benefit and service data.
- Phase implementation: Pilot one or two APIs in a controlled environment before scaling.
- Align with other initiatives: If you’re already undergoing portal upgrades or EHR integration work, combine efforts to minimize disruption.
Pitfall to avoid: Waiting until late 2026 to start — APIs that touch multiple external systems require longer lead times.
mPulse POV: Build your roadmap backward from January 1, 2027, but front-load high-value APIs so you can start realizing benefits before the mandate.
4. Engage Vendors Early
Third-party platforms are often the linchpin for meeting these requirements.
- Ask about compliance roadmaps now: Vendors should be able to outline their development timelines.
- Clarify integration models: Will they handle the API hosting, or will you?
- Negotiate support for adoption: Ensure vendors will assist with provider onboarding and training.
Pitfall to avoid: Assuming vendors are automatically building these capabilities.
mPulse POV: As a portal vendor with proven FHIR API implementation experience, we can streamline this process by integrating directly into the tools your providers already use.
5. Plan for Adoption, Not Just Implementation
Launching the APIs isn’t enough — they have to be used to deliver value.
- Provider training: Offer webinars, short video demos, and step-by-step guides.
- Member communication: Explain how faster prior auth decisions benefit them directly.
- Measure utilization: Track which providers are using the APIs and where additional outreach is needed.
- Close the feedback loop: Continuously refine workflows based on feedback.
Pitfall to avoid: Declaring success at go-live without adoption metrics.
mPulse POV: We build education and usage tracking into our solutions so plans can see — and demonstrate — the real-world impact.
Strategic Outlook: Turning Compliance Into Competitive Advantage
While CMS-0057F is rooted in regulation, forward-looking plans are treating it as a digital health transformation initiative. Here’s why:
- Market Shifts: Federal pledges to streamline prior auth suggest these standards could extend to commercial markets.
- Brand Reputation: Public reporting of turnaround times, approval rates, and volumes will influence how providers and members perceive your organization.
- Operational Leverage: The APIs create datasets that can fuel predictive analytics, care management, and member engagement strategies.
- Experience Differentiation: Imagine marketing your plan as the one that consistently approves requests faster, with fewer denials and less back-and-forth.
By reframing CMS-0057F as a foundation for future capabilities, you transform a compliance requirement into an investment in long-term growth.
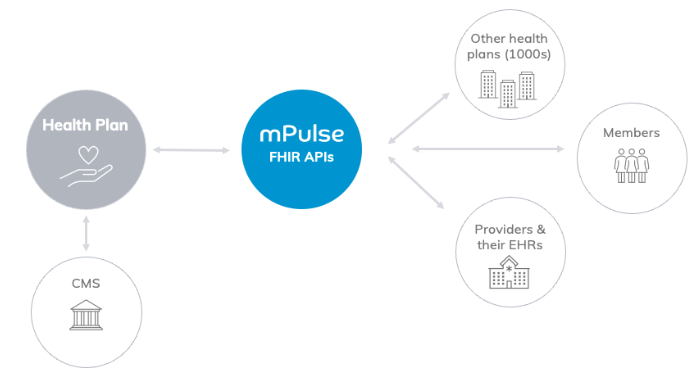
How mPulse Supports You
mPulse is already working with health plans to:
- Leverage Proven Foundations – Building on our experience implementing the CMS-9115F APIs.
- Deliver Self-Service Reporting – Tools to generate CMS-facing and public-facing metrics.
- Enable Education & Adoption – Provider and member templates to increase API utilization.
- Integrate Seamlessly – Embedding APIs within your existing portal ecosystem.
Conclusion: Start Now to Lead Later
CMS-0057F is more than a checklist — it’s a catalyst for innovation in interoperability, transparency, and prior authorization.
By starting now, you can:
- Avoid last-minute risks.
- Build trust with providers and members.
- Use compliance as a springboard for strategic advantage.
mPulse is here to partner with you on every step of this journey. Let’s turn regulation into an opportunity for faster care, less friction, and better outcomes for all.
Frequently Asked Questions (FAQ)
What is CMS-0057F?
CMS-0057F is a final rule from the Centers for Medicare & Medicaid Services focused on interoperability and prior authorization. It introduces faster prior authorization decision timelines, denial reason transparency, new reporting requirements, and the implementation of five new FHIR APIs by January 1, 2027.
Who does CMS-0057F apply to?
The rule applies to state Medicaid and CHIP agencies, Medicaid and CHIP managed care plans, Medicare Advantage organizations, and Qualified Health Plan issuers on federally facilitated exchanges. Even commercial health plans not directly required may benefit from preparing early.
What are the key deadlines for CMS-0057F?
- 2025: New prior authorization decision timelines and denial transparency requirements.
- 2026: Public-facing reporting of prior authorization metrics and CMS-facing reporting on Patient Access API usage.
- 2027: Implementation of five new FHIR APIs.
Which FHIR APIs are required by CMS-0057F?
The five required APIs are:
- Provider Access API
- Payer-to-Payer API
- Coverage Requirements Discovery API
- Documentation Templates & Rules API
- Prior Authorization Support API
What changes are required for prior authorization under CMS-0057F?
Health plans must meet faster decision timelines: 7 calendar days for standard requests, 72 hours for expedited requests, and 24 hours for urgent cases. They must also provide clear denial reasons and make prior authorization metrics publicly available.
How should health plans prepare for CMS-0057F?
Plans should begin by auditing their current processes, forming a cross-functional task force, prioritizing their implementation roadmap, engaging vendors early, and planning for provider adoption and training.





