7 Ways to Meet Healthcare Consumers Online and Boost Your Member Experience
“Healthcare consumerism” – it’s a buzzword heard a lot over the past few years as the healthcare industry has evolved to be more consumer-centric, and all healthcare professionals should know and understand it. Patients are taking a more proactive role in their own health and wellness (long overdue), acting as purchasers and turning to digital solutions for quick and convenient access to healthcare information, products and care. As consumers, they now demand more control and responsibility for selecting the right health plan that best fits their needs and the needs of their families. Once a member, they want relevant and timely information regarding their plan and benefits at their fingertips.
It’s important to ensure health plans are providing the support and resources needed for healthcare consumers to make educated and informed decisions about their health and benefits.
The first question to ask: what are the key resources to provide?
1. A Digital Front Door
In a recent article, Advisory Board identified four main goals of the digital front door:
- improve satisfaction with a simplified member experience
- expand access to care
- optimize resource allocation (often through self-service tools)
- reduce unnecessary treatment through better care coordination
For these reasons, investing in digital front doors should be the highest priority for health plans and other healthcare organizations. Consumers today expect a digital experience in many elements of their lives, and their health is no exception.
To achieve these goals, health plans can focus on providing digital resources through their portals, such as care team messaging, helpful chatbots, pre- and post-visit or operation educational resources, disease management tools, and online premium payments. The more a member can do online and through their portal, the happier they are as a healthcare consumer.
2. Omnichannel Digital Engagement
Omnichannel engagement strategies are used by successful brands to lure customers, learn about their behaviors, and drive loyalty. They allow brands to create a series of touchpoints and to reach people through their preferred channels. Obsolete methods of communication, such as direct mail, lack personalization and the ability to collect data at scale.
When healthcare organizations use omnichannel digital engagement, they are able to reach consumers in the way they prefer and provide a more enjoyable member or patient experience. Without an omnichannel communication strategy, it’s impossible to effectively deliver appropriate resources and education to a broad member database.
Below are just a few examples of digital ways to engage and activate more consumers and engage them about impactful topics that have significant impact on the member experience.
- Interactive voice response (IVR)
- Mobile web
- Short message service (SMS)
- Multimedia message service (MMS)
- Rich communication services (RCS) channels
3. Tailored Plan Shopping
Each healthcare consumer has a unique set of needs to be met and features that are important to them when searching for a health plan. Desired monthly premiums, copay and deductible amounts, in-network doctors, hospitals, and other health care providers, chronic illness support, and so much more. Searching through and finding the right health plan based on all of these things can be an overwhelming and complicated process.
According to the 2023 KFF Survey of Consumer Experience with Health Insurance, nearly one in three adults with Marketplace coverage (31%) found it very or somewhat difficult to compare copays and deductibles under their plan options, and one in four (25%) found it very or somewhat difficult to compare monthly premiums.
Simplify the plan shopping process through an intuitive questionnaire that gathers information from the consumer that can then be used to present them with the health plan that makes the most sense. Taking the burden off the consumer to do the hard work boosts their confidence in making the right selection and will lead to higher member satisfaction down the road.
4. Provider Search
Consumers spend a lot of time online researching practices, providers, and more. In fact, more than 3 in 4 patients (77%) look for doctors online often according to Tebra’s 4th annual Patient Perspectives survey. One of the top places patients start looking is their online insurance directories, with 53% of patients saying online insurance directories contribute to their doctor selection decision.
Providing correct and updated information for all providers, as well relevant search filters such as location, type of provider, gender, language spoken, and whether they are accepting new patients, are helpful in a consumer’s search. The easier you can make it for a member or potential member to find the information they need, the happier they will be with their health plan experience.
5. Price Transparency Tool
Health plan price transparency tools help consumers know the cost of care or service before seeing a provider. The State of Patient Access 2023, completed by Experian Health, found that:
- 65% of patients said they did not receive an estimate prior to care, with 41% of those respondents said final costs were more than expected
- 40% of all patient respondents said they were likely to cancel or postpone care without an accurate estimate
- 79% of all patient respondents say an accurate estimate helps them better prepare to pay care costs
- 88% said receiving a price estimate before care is important
Not having the cost estimates they need is leading healthcare consumers to defer treatment and avoid the care they need, leading to increased hospitalization and complications from preventable diseases.
By providing a price transparency tool and giving members the opportunity to access this information before a visit, procedure, or purchase, health plans are giving consumers the ability to make informed decisions that best meet their needs and financial situation and help improve health outcomes.
6. Easy-to-Understand Member Statements and Benefits Overview
A recent KFF Survey of Consumer Experiences with Health Insurance asked insured adults about how well they understand key aspects of their health insurance. Half (51%) of insured adults say they find at least one aspect of how their insurance works at least somewhat difficult to understand.
These items caused the most confusion:
- What insurance covers – More than one-third (36%) of all insured adults say it is at least somewhat difficult for them to understand what their insurance will and will not cover
- Out-of-pocket costs – Thirty percent of insured adults overall say it is difficult for them to understand what they will owe out-of-pocket when they get health care
- Explanation of Benefits (EOB) – Three in ten insured adults say they find it difficult to understand whether or how much insurance will pay for care from looking at their EOB
- Basic health insurance terminology – A quarter of all insured adults say they have difficulty understanding specific terms, such as “deductible,” “coinsurance,” “prior authorization,” or “allowed amount.”
Health plans can alleviate this confusion by providing resources that help their members understand their coverage. Through the member portal, plans should show up-to-date information regarding what is available to members with their benefits or even plan discounts, explain and outline their deductible and out-of-pocket maximums in a member-friendly manner, and inform them of their benefit accumulators for both in-network and out-of-network services. Using a built-in glossary to define key terminology can also help members as they sort through the information being presented to them.
7. Member and Patient Education
One major factor impacting the member and patient experience is health literacy. With 35% of the adult US population having basic or below basic health literacy, education is vital to ensuring a positive member or patient experience.
To combat the health literacy challenge, the healthcare industry must reimagine what member and patient education looks like. Healthcare consumers are, at the end of the day, simply consumers, and consumers ingest content and information continuously every day from a multitude of sources: short, bite sized videos on social media, streaming services for shows and movies, a large volume of self-produced content, and more.
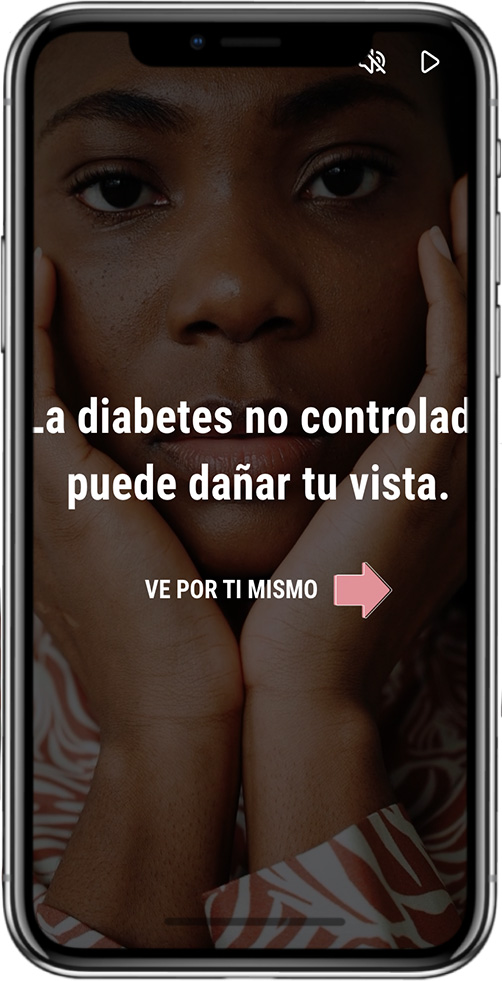
Taking inspiration from all around us and applying it to member and patient education means engaging with healthcare consumers in the ways they are showing us they like, enjoy, and want. When engaging with members, you can send short, bite sized videos on why getting vaccinated from the flu is important or a full course they can stream to learn about managing their diabetes.
And this type of streaming health content has proven to be an effective method of capturing the health consumer’s attention. One large national plan which partnered with mPulse on digital outreach saw a 274% increase in link clicks to schedule their annual eye exam when this video was utilized vs when no video was sent.
Getting Started
The second question to ask: why should a health plan make the commitment and investment to provide these resources?
Health plans who implement these tools for their members can gain:
- Increased member acquisition and retention
- Higher member satisfaction
- Operational efficiency
- Competitive advantage
How can health plans get started if they already aren’t doing these things?
Reach out to mPulse to learn more about our product offering and how we can help you answer the demand for healthcare consumerism. Our products are built to provide your members with the resources they need to be educated, informed, and proactive about their health.
Article originally published on healthtrio.com.






