Introduction
Medicare Advantage plans have had several months to review the 2025 Star Ratings as well as the recently recalculated release. Performance trends continue to highlight a competitive and rapidly evolving landscape for Medicare Advantage and Prescription Drug Plans (MA-PD) in the coming years. With new CMS policies taking effect, cut point trends, methodological changes, and a growing Medicare beneficiary population, MA-PD plans must adopt strategic and innovative approaches in 2025 to navigate the industry’s increasing demands and complexities.
2025 Star Key Observations
- 9 plans received five stars in 2025, down from 38 in 2024
- 40% of plans received four or more stars, down from 68% in 2022 (source)
- 62% of MA-PD enrollees (by enrollment weight) are currently in a plan that will have four or more stars in 2025
- 3.92 MA-PD average Star Rating continues a steady decline from prior years (4.07 for 2024 and 4.14 for 2023)
2026 Star Ratings Key Changes
Heightened competition, reduced bonus payments, and the upcoming Part D changes will push plans to focus on cost-containing measures and strategic initiatives targeting higher-weighted metrics.
New Measure
For 2026 Stars, we will see the addition of only one new measure, Kidney Health Evaluation for Patients with Diabetes that officially replaces the now retired Diabetes Care – Kidney Disease Monitoring measure.
Returning Measures
The two longitudinal measures from the Health Outcomes Survey (HOS) Improving or Maintaining Physical Health and Improving or Maintaining Mental Health will return from the display page with a weight of 1x each for the first year before increasing to 3x each for subsequent Stars years.
Weight Changes
Patient experience, complaints, and access measures will drop from 4x each to 2x each while still accounting for a significant portion of the overall summary rating. Upcoming Part D cost share changes will be favorable to beneficiaries ($2000 max out of pocket and the removal of the coverage gap) but the shift in cost share to plans has resulted in additional utilization management, increased prevalence of Part D deductibles, formulary changes and more. Managing member expectations and ensuring appropriate access to prescription drugs in the 2025 plan year will have a direct impact on these measures.
Strategies for Success
Plans should focus on triple weighted measures that are also seen as a force multiplier across general measure sets and both QI measures. Focusing continued improvement across Diabetes Care – Blood Sugar Controlled, Controlling Blood Pressure, Plan All-Cause Readmissions, Medication Adherence for Diabetes, Hypertension, and Cholesterol will have a significant impact on overall ratings as well as the upcoming Health Equity Index and Reward (2027 Stars).
The Correlation in Performance between Measure Categories
Process, outcomes, experience and access measures, while categorized separately, are profoundly interconnected, with performance and compliance often being tied to a member’s self-efficacy. When members feel like an equal partner in their care and have the right tools and support to feel empowered, they’re often more satisfied with their care and have a better perception of their plan and better health outcomes.
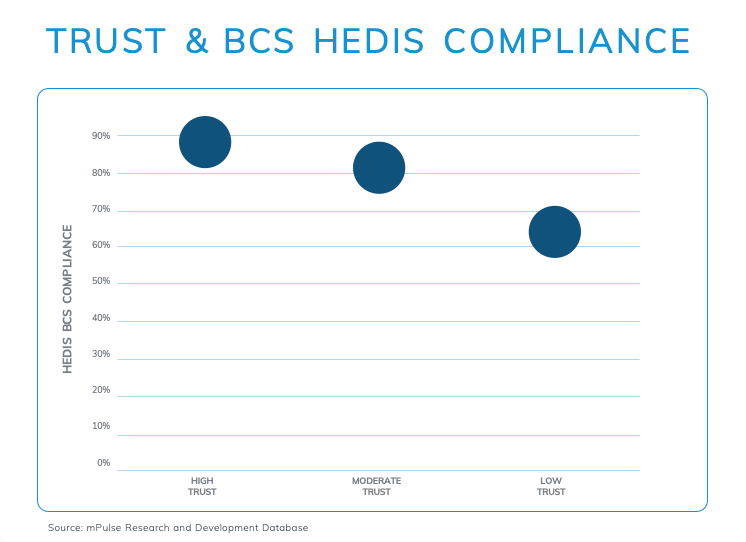
Below is an example of Breast Cancer Screening (BCS) screening rates among high, moderate and low trust member cohorts. Src: mPulse Research and Development Database.
To learn more about the impact of trust on quality performance and member satisfaction, watch our on-demand Webinar, Talking CAHPS: Member Trust Edition.
Looking Ahead: Strategies for Improving Star Ratings Performance
With an increased need to protect costs and implement innovative strategies to improve performance for the years ahead, plans will need to harness innovate technology such as artificial intelligence (AI) and Machine Learning (ML) to automate manual processes and reduce administrative costs. The ability to show value, both qualitative and quantitative across departments and internal stakeholders will also become imperative as budgets are scrutinized, and the need to increase member health and experience outcomes increases.
Harnessing AI and Technology
In a fast-paced and highly competitive environment, health plans continually look to form partnerships with third party vendors that offer scalable AI solutions that solve their most pressing challenges. Decision Point Insights is an easy-to-navigate application that enables health plans to view both population-wide and member-level insights and predictions using 100+ predictive models. Our predictive models are continuously enhanced to deliver proven predictions that allow health plans to segment their population by risk based on one or more attributes or measures, enabling proactive, data-driven decision making with timely and relevant interventions.
Consolidating Resources & Protecting Costs
The reduction in bonus payments and higher cut points has also led to a decline in some benefit offerings for beneficiaries, including over-the-counter, meal, remote technologies, transportation, and more. The reduction of resources is an indicator of changing budgets, which further highlights the need for plans to implement solutions that cut unnecessary spending, improve operational efficiencies and improve member health outcomes and satisfaction. The average health plan spends approximately $14M operating a call center and upward of 10%+ of their budget to direct mail annually. mPulse Activators are ready-to-go proven omnichannel engagement programs designed to improve member health outcomes across star performance categories. Our programs leverage conversational AI to decipher complex member responses and follow-up with the right tools and support at key moments to empower health action.
Example: With HOS measures returning for 2026 Stars and increasing in weight for 2027 and beyond, leveraging predictive models to assess risk scores, and then deploying targeted HOS Activator programs to build member self-efficacy and health perception at scale is critical for protecting costs and improving outcomes.
Check out mPulse’s Outcomes Tied to 3X weighted Star Measures:
» 11.78pp improvement in CBP compliance rates compared to control group
» 7.71pp Improvement in CDC HbA1c Controlled compared to control group
» 65% decrease in the number of calls needed to reach a member for post-discharge follow-up care plan
» 3.5pp improvement in YoY Part D medication adherence rates
Compare your 2024 and 2025 Star Ratings performance by domain using our Star Compare tool. For deeper insights into your 2025 performance and tailored recommendations to optimize for 2026 and beyond, request a personalized Star Report and consultation with our quality performance expert, Reva Sheehan.

2025 Stars Compare Tool
15 Oct 2024 | 5 min read
Get Your Custom Report ≫