In healthcare, engaging health consumers effectively is becoming increasingly complex. Health plans, providers, hospital systems, and pharmacies deploy various communication strategies – from emails and text messages to phone calls and live events – all to motivate health consumers toward better health decisions. However, the key to capturing attention and prompting action often lies in overcoming knowledge, skill, or motivation gaps. This is where streaming health education, a nuanced form of digital health content, emerges as a vital tool.
But getting someone to stop, pay attention, and act can be challenging. There are many barriers that stand in the way. When one or more of those barriers reflects knowledge, skill, or motivation gaps, streaming health education might supply the nudge that helps move them in the right direction.
Streaming health content, a sophisticated approach to health literacy, merges the strengths of digital content strategy, behavioral science, and instructional design to craft impactful learning experiences. It’s not just about delivering information; it’s about engaging health consumers through diverse formats like animated videos, interactive activities, and expert-led courses. This post delves into seven innovative ways healthcare organizations can harness streaming health content to drive critical health behaviors, starting with the captivating storytelling format of fotonovelas.
As we navigate the ever-evolving landscape of digital health content, it’s clear that the right health content can educate and empower consumers, leading to better health outcomes and adherence to care plans.
Nudging your members to act with streaming health education
What is streaming health education? It’s our take on health literacy promotion. It borrows from the best of digital content strategy, behavior science, and instructional design to create powerful learning experiences for your members.
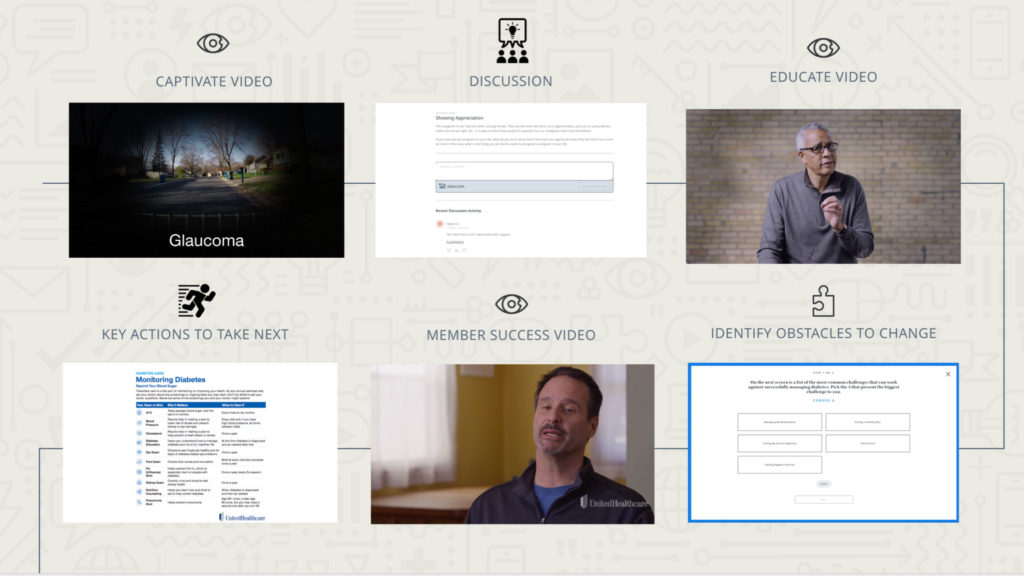
From short, animated videos and interactive activities to media-rich online lessons and courses taught by leading health experts, there are many different and innovative ways to create and provide content to your health consumers.
In this post, we break down 7 ways healthcare organizations can use digital health content in their engagement programs to drive essential health behaviors, starting with fotonovelas.
Use Fotonovelas to Encourage Flu Vaccinations
Over 3 million Americans get the flu yearly, and the cost to the healthcare system and society in general adds up to a whopping 11.2 billion dollars a year. This is a great reason to educate members on flu vaccinations, which can be done well through fotonovelas, which are character-based stories told through photos or illustrations.
 In this flu fotonovela, which is one of the four included in our flu vaccination solution, health consumers are educated on why a flu shot matters and common barriers and misconceptions related to flu vaccination. At the end, they’re given an easy resource for scheduling their shot.
In this flu fotonovela, which is one of the four included in our flu vaccination solution, health consumers are educated on why a flu shot matters and common barriers and misconceptions related to flu vaccination. At the end, they’re given an easy resource for scheduling their shot.
It’s ultimately a health literacy tool, but at the same time, it makes learning fun and easy. Behavioral Strategist, Eden Brownell, explained the reason for the success of fotonovelas on the Pharmacy Friends podcast. “The perceived effort is lower. You can provide a large amount of information in a large text message, or you can bundle it up into a fotonovela. [In a fotonovela] it’s broken up. They’re able to see the progression they’re making through the story, which provides them with a sense of accomplishment, and the way it’s being delivered feels easier. When people feel that something is easier, they’re more likely to like it.”
And we find that fotonovelas are certainly well-liked. 80% of learners on our platform report liking or loving the fotonovela content type.
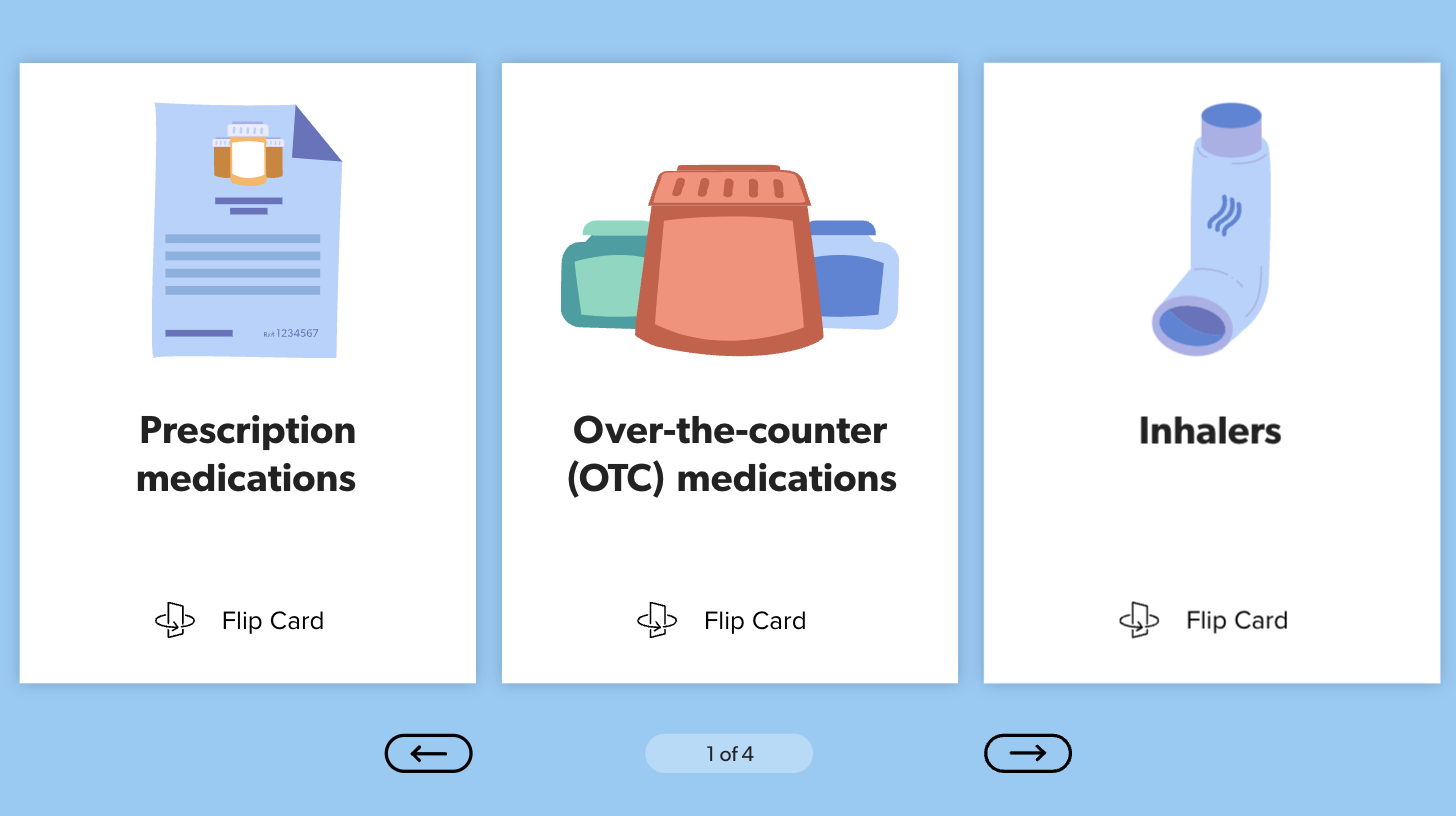
Interactive Content to Promote Medication Adherence
20-30% of medication prescriptions are never filled. Almost 50% of prescriptions are not taken as prescribed. It’s hard for a medicine to work of you don’t take it.
But then again, it’s hard to get your members to abide by their medication regimen if you aren’t addressing barriers to compliance and educating them on the importance of medication adherence. That’s where our second content piece comes in.
Interactive content can do well to educate and motivate health consumers to follow through on their prescriptions. In this series of interactive activities, members gain important knowledge on why and how to follow this critically important part of their care plans – all easily integrated into med adherence and medication management campaigns.
When the member or patient arrives at the interactive content, they can decide which barrier or medication type applies to them and read through the information at their own pace skipping anything they don’t feel addresses their specific situation. And a program like this with content infused has been shown to increase refill rates by 14%!
Using Animations to Educate on the Proper Use of the ER
A recent study from UnitedHealth Group estimated that members going to the emergency room for non-emergencies costs the health system $32 billion annually. Ouch.
But a short video on the proper use of urgent care versus emergency rooms is an excellent example of utilizing animations to educate your health consumers. Able to be sent through text or email or placed on a website or portal, animations are a fun and engaging way to educate. This animation is a prime example of education leading to reduced cost and better healthcare decisions for both the member and the plan, and it’s also highly likely to get your members chuckling. Watch the below animation to see what we mean!
In Part 2…
Health content is aimed at driving healthy actions and educating someone on why those actions should be taken. It addresses health literacy at the same time as it enables plans and providers to reach their own goals.
In part 2, we’ll tackle the next four ways to integrate content into your outreach: lessons, expert-led courses, self-assessments, and stories.